When the Liver Is the Target


Articles in Hematopoiesis are written for trainees by trainees, under the oversight of the ASH Trainee Council. The material published in Hematopoiesis is for informational purposes only. The opinions of the authors are their own and do not necessarily represent the official policy of the American Society of Hematology. ASH does not recommend or endorse any specific tests, physicians, products, procedures, or opinions, and disclaims any representation, warranty, or guarantee as to the same. Reliance on the information provided in this publication is solely at your risk.

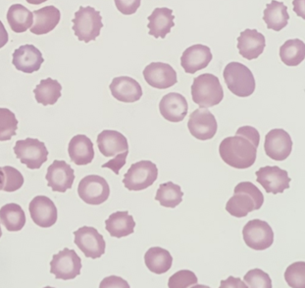
A 74-year-old woman with alcohol use disorder presented to the emergency department with alcohol withdrawal and diarrhea. She was treated with phenobarbital for alcohol withdrawal and vancomycin for Clostridium difficile infection. On the second day of admission, her platelets were 216 × 103/µL with normal liver function tests. One day later, her platelet count decreased to 9 × 103/µL, at which time hematology was consulted. Laboratory values showed alanine aminotransferase at 178 U/L, aspartate transferase was 1,552 U/L, total bilirubin 2.5 mg/dL, direct bilirubin 1.9 mg/dL, prothrombin time (PT) was 37.8 seconds, international normalized ratio was 4.0 mg/dL, activated partial thromboplastin time (aPTT) 45.3 seconds, D-dimer more than 4,000 ng/mL, and fibrinogen was 110 mg/dL. The peripheral blood smear demonstrated echinocytes, target cells, and schistocytes concerning for acute liver injury and disseminated intravascular coagulation (DIC; Figure 1 at 50× and Figure 2 at 100×). Echinocytes form due to binding of high-density lipoproteins to red blood cell surfaces,1 target cells form due to abnormal lipid deposition, and schistocytes occur due to microvascular shearing from abnormal fibrin deposition. Echinocytes (also called burr cells) have regular spicules and are more commonly seen in renal disease but can also be observed in liver disease as in this case. Echinocytes should be differentiated from acanthocytes (also called spur cells), which have more irregular projects and are more commonly found in liver disease. Schistocytes were present at about one to two schistocytes per high power field; this is fewer schistocytes than would be normally seen in a thrombotic microangiopathy.
Figure 1. Peripheral blood smear at 50×
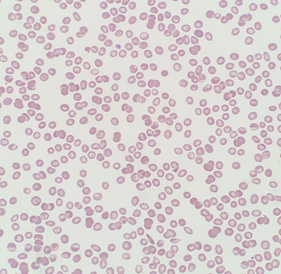
Figure 2. Peripheral blood smear at 100×
Despite an extensive infectious, inflammatory, and toxicology workup, no etiology for acute liver injury was clearly identified, although recent antibiotic use prior to hospitalization was possible. She received cryoprecipitate to achieve a fibrinogen higher than 150 mg/dL due to evidence of colitis-associated bleeding. Liver disease can also lead to dysfibrinogenemia, so this may have been a factor in her case as well. Given the critical contribution of fibrinogen to the common pathway, cryoprecipitate will often correct mild prolongations in coagulation times, which is what occurred in this case with normalization of her PT and PTT after cryoprecipitate. For severe fibrinogen deficiency, fibrinogen concentrate can be given instead of cryoprecipitate. If the PT or PTT remain greater than two times the upper limit of normal despite correcting the fibrinogen deficit, fresh frozen plasma may be given. She did not experience further bleeding and her laboratory values improved over the following three weeks.
- Owen JS, Brown DJ, Harry DS, et al. Erythrocyte echinocytosis in liver disease. Role of abnormal plasma high density lipoproteins. J Clin Invest. 1985;76:2275-2285.
Dr. Zon is a consultant for and has equity ownership in Amagma Therapeutics. Dr. Connell is a consultant and board or advisory committee member for Takeda, has equity ownership in Doximity, and is a board or advisory committee member for the Michael H. Flanagan Foundation.