When It Isn’t ITP: A Case Presentation



Articles in Hematopoiesis are written for trainees by trainees, under the oversight of the ASH Trainee Council. The material published in Hematopoiesis is for informational purposes only. The opinions of the authors are their own and do not necessarily represent the official policy of the American Society of Hematology. ASH does not recommend or endorse any specific tests, physicians, products, procedures, or opinions, and disclaims any representation, warranty, or guarantee as to the same. Reliance on the information provided in this publication is solely at your risk.
 A 74-year-old man with a previous diagnosis of immune thrombocytopenia purpura (ITP) in 2018 presented to the hematology clinic for an evaluation of severe isolated thrombocytopenia, which did not improve following a four-day course of dexamethasone 40 mg. At the time of assessment, he reported experiencing easy bruising but denied spontaneous bleeding. He was otherwise well without constitutional symptoms. He had no personal or family history of bleeding disorders or malignancy. His physical exam revealed mild wet and peripheral purpura; there was no lymphadenopathy, splenomegaly, or stigmata of chronic liver disease.
A 74-year-old man with a previous diagnosis of immune thrombocytopenia purpura (ITP) in 2018 presented to the hematology clinic for an evaluation of severe isolated thrombocytopenia, which did not improve following a four-day course of dexamethasone 40 mg. At the time of assessment, he reported experiencing easy bruising but denied spontaneous bleeding. He was otherwise well without constitutional symptoms. He had no personal or family history of bleeding disorders or malignancy. His physical exam revealed mild wet and peripheral purpura; there was no lymphadenopathy, splenomegaly, or stigmata of chronic liver disease.
His medical history included benign prostatic hypertrophy, dyslipidemia, hypertension, alcohol use disorder, and psoriasis. His active medications consisted of dutasteride, atorvastatin, irbesartan, and ixekizumab (anti-IL17A monoclonal antibody, which was initiated four months before presentation). He reported drinking two vodka beverages per day for the past decade.
An abdominal ultrasound demonstrated fatty liver with no evidence of cirrhosis and a normal splenic diameter of 8.4 cm. Laboratory results are shown in the Table.
Table 1. Initial Laboratory Investigations
| Lab Values | Result | Reference Range |
| White blood cell (WBC) | 10 × 109/L (normal differential) | 4-11 × 109/L |
| Hemoglobin (Hbg) | 133 g/L | 135-170 g/L |
| Platelets | 9 × 109/L | 150-450 × 109/L |
| International normalised ratio (INR) | 1 | 0.9-1.2 |
| Partial thromboplastin time (PTT) | 23 sec | 21-29 sec |
| Creatinine | 69 μmol/L | 0-110 μmol/L |
| Total bilirubin | 11 μmol/L | 0-17 μmol/L |
| Alanine aminotransferase (ALT) | 28 U/L | 8-45 U/L |
| Alkaline phosphatase (ALP) | 66 U/L | 64-133 U/L |
| Albumin | 35 g/L | 35-48 g/L |
| B12 | 288 pmol/L | 138-652 pmol/L |
| Ferritin | 141 μg/L | 22-275 μg/L |
| Antinuclear antibody (ANA) | Negative | Negative |
| Complement component 3 (C3) | 1.37 g/L | 082-1.85 g/L |
| Complement component 4 (C4) | 0.3 g/L | 0.13-0.4 g/L |
| HIV | Non-reactive | Non-reactive |
| Hepatitis C virus (HCV) | Non-reactive | Non-reactive |
| H. pylori serology | Negative | Negative |
| COVID-19 polymerase chain reaction (PCR) | Negative | Negative |
| Peripheral smear | Isolated severe thrombocytopenia, no platelet clumping, no dysplastic changes, no fragments |
The most likely diagnosis for this man with severe isolated thrombocytopenia at that time was ITP.1 Due to challenges in accessing second-line treatments for ITP in Canada, the patient was treated with prednisone 1 mg/kg/day. He was also advised to taper off alcohol to which he complied. After two weeks of steroid unresponsiveness, he was advanced to a two-day course of intravenous immune globulin (1 g/kg/day). His platelet counts are shown in Figure 1.
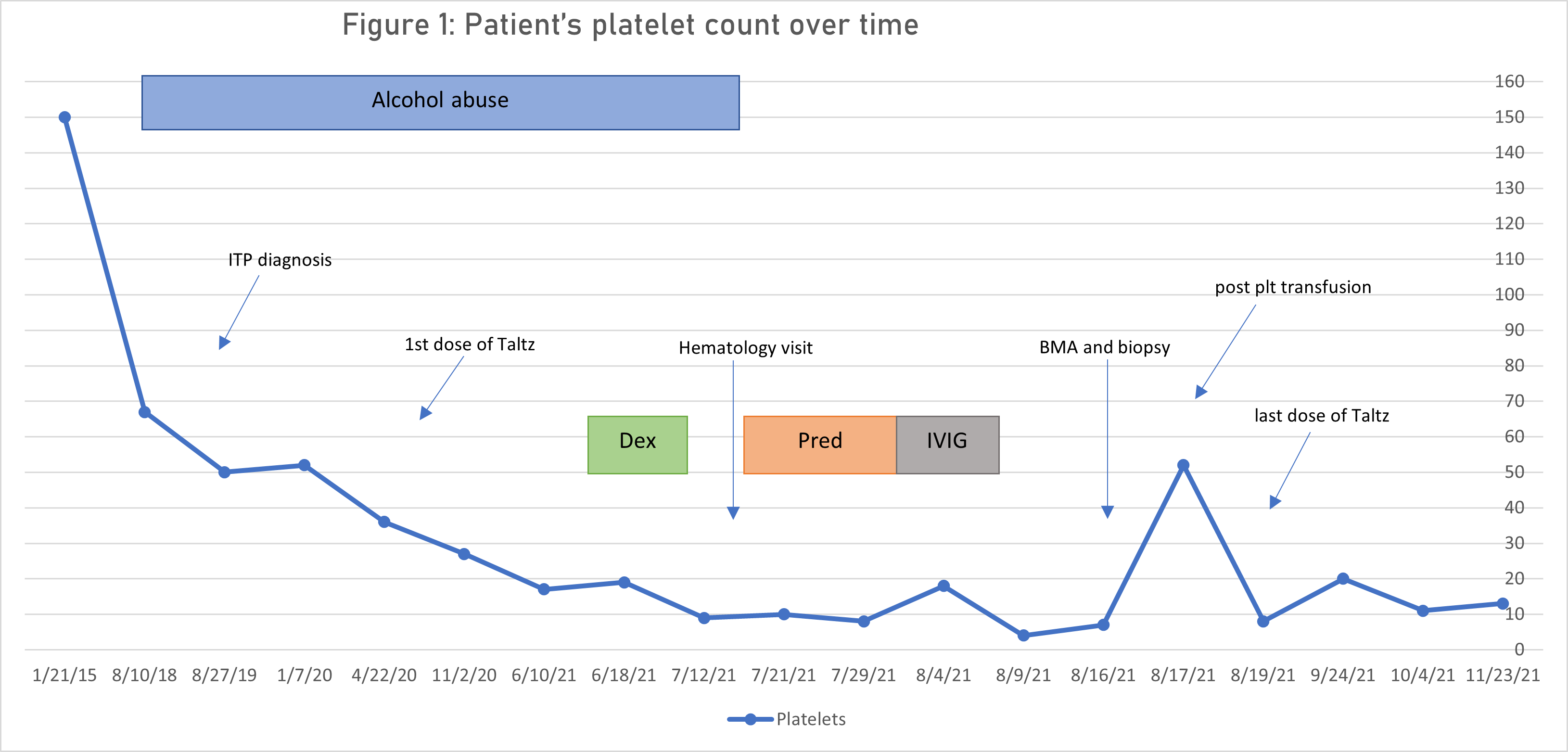
Abbreviations: BMA, bone marrow aspirate; Dex, dexamethasone; ITP, immune thrombocytopenia purpura; IVIG, intravenous immune globulin; plt, platelet; Pred, prednisone; Taltz, ixekizumab.
Differential Diagnosis of Refractory ITP
DITP is a clinical diagnosis that requires a high index of suspicion and a thorough review of the patient’s drug history. Although our patient was not taking any medications frequently associated with thrombocytopenia (www.ouhsc.edu/platelets), his new anti-IL17A monoclonal antibody was temporally related to a rapid decline in his platelets. Laboratory testing for DITP is possible at select laboratories; however, the utility of such tests is low because negative controls may not exist, or a drug’s metabolite may be implicated.3 The diagnosis of DITP is confirmed when thrombocytopenia resolves, usually in one to two days after stopping the offending agent.3
MDS with single lineage dysplasia should be considered because the incidence of MDS increases with age. Although uncommon, MDS can present with isolated thrombocytopenia in approximately 10 percent of patients.4
Acquired amegakaryocytic thrombocytopenia (AAT) is a rare disorder characterized by isolated thrombocytopenia that results from a paucity of megakaryocytes in an otherwise normal bone marrow.5 This is in contrast to ITP where a preponderance of megakaryocytes is usually observed. The prevalence of AAT is unknown because the literature is limited to case reports.5 Although the exact mechanism of AAT remains unclear, it is strongly suspected to be related to immune dysregulation. Studies have demonstrated cell-mediated inhibition of megakaryocytes, possibly by monocytes or a clonal population of T-lymphocytes,6 as well as a presence of anti-thrombopoietin (TPO) and anti-cMpl autoantibodies.7 Peripherally, AAT and ITP are indistinguishable, which underscores the importance of a bone marrow examination in cases of refractory ITP.
Case Continuation
On August 16, the patient underwent a bone marrow aspirate and biopsy (Figure 1); cytogenetic analysis was not performed. The patient also received a transfusion of one unit of pooled platelets, which resulted in a nonsustained 45-point platelet increment at 24 hours (Figure 2). His ixekizumab was discontinued on August 19. His platelet levels remained in the range of 10 to 20 × 109/L for the following three months (Figure 1).
Figure 1. Patient’s Bone Marrow Aspirate and Biopsy
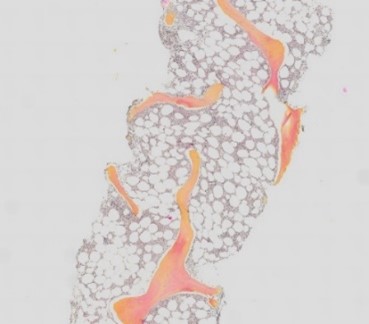 |
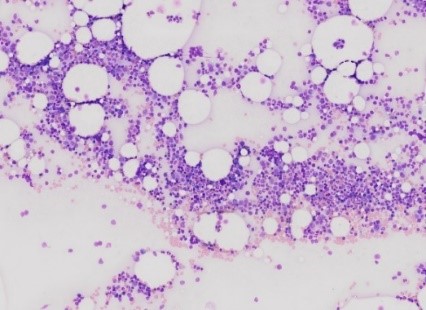 |
Figure 2. Bone Marrow Biopsy
Bone marrow core biopsy (magnified with 3× objective; left) and aspirate (magnified with 10× objective; right) show normocellular marrow with a paucity of megakaryocytes but no other abnormalities.
Case Continuation
The patient’s viral studies were non-reactive. He also had an unremarkable CT C/A/P. Cytogenetic and molecular studies on the repeat bone marrow examination are pending. He presented to the office wishing to discuss other treatment options for his idiopathic AAT given ongoing mild mucocutaneous bleeding. Oral TPO agonist eltrombopag was initiated based on case reports of efficacy and a favorable adverse effect profile compared to immunosuppressants in older patients.16 Evaluation of his response to eltrombopag is ongoing.
- Neunert C, Terrell DR, Arnold DM, et al. American Society of Hematology 2019 guidelines for immune thrombocytopenia. Blood Adv. 2019;3:3829-3866.
- Miltiadous O, Hou M, Bussel JB. Identifying and treating refractory ITP: difficulty in diagnosis and role of combination treatment. Blood. 2020;135:472-490.
- Arnold DM, Nazi I, Warkentin TE, et al. Approach to the diagnosis and management of drug-induced immune thrombocytopenia. Transfus Med Rev. 2013;27:137-145.
- Waisbren J, Dinner S, Altman J, et al. Disease characteristics and prognosis of myelodysplastic syndrome presenting with isolated thrombocytopenia. Int J Hematol. 2017;105:44-51.
- Agarwal N, Spahr JE, Werner TL, et al. Acquired amegakaryocytic thrombocytopenic purpura. Am J Hematol. 2006;81:132-135.
- Gewirtz AM, Sacchetti MK, Bien R, et al. Cell-mediated suppression of megakaryocytopoiesis in acquired amegakaryocytic thrombocytopenic purpura. Blood. 1986;68:619-626.
- Kuwaki T, Hagiwara T, Kato T, et al. Autoantibodies neutralizing thrombopoietin in a patient with a megakaryocytic thrombocytopenic purpura. Blood. 2000;95:2187-2188.
- Lugassy G. Non-Hodgkin’s lymphoma presenting with amegakaryocytic thrombocytopenic purpura. Ann Hematol. 1996;73:41-42.
- Griner PF, Hoyer LW. Amegakaryocytic thrombocytopenia in systemic lupus erythematosus. Arch Intern Med. 1970;125:328-332.
- Bhattacharyya J, Kumar R, Tyagi S, et al. Human parvovirus B19-induced acquired pure amegakaryocytic thrombocytopenia. Br J Haematol. 2005;128:128-129.
- Maslovsky I, Gefel D, Uriev L, et al. Malignant thymoma complicated by amegakaryocytic thrombocytopenic purpura. Eur J Intern Med. 2005;16:523-524.
- Ghosh K, Sarode R, Varma N, et al. Amegakaryocytic thrombocytopenia of nutritional vitamin B12 deficiency. Trop Geogr Med. 1988;40:158-160.
- Gewirtz AM, Hoffman R. Transitory hypomegakaryocytic thrombocytopenia: aetiological association with ethanol abuse and implications regarding regulation of human megakaryocytopoiesis. Br J Haematol. 1986;62:333-344.
- Font J, Nomdedeu B, Martinez-Orozco F, et al. Amegakaryocytic thrombocytopenia and an analgesic. Ann Intern Med. 1981;95:783.
- Al Pakra M, Al Jabri A, Hanafy E. Myelodysplastic syndrome presenting as amegakaryocytic thrombocytopenia in a collodion baby. J Investig Med High Impact Case Rep. 2015;3:2324709615605637.
- Roy AM, Konda M, Sidarous GK, et al. Acquired amegakaryocytic thrombocytopenia misdiagnosed as immune thrombocytopenia: A case report. Perm J. 2020;24:1-3.