Image Challenge: Hematology Consult - Middle-Age Woman With Neutropenia and Splenomegaly
A 47-year-old female with a history of anti-cyclic citrullinated peptide (anti-CCP) and rheumatoid factor sero-positive rheumatoid arthritis was sent to your outpatient clinic with a diagnosis of neutropenia. She has not had any recent infections. Her rheumatoid arthritis mainly affects her hands and has been under control with etanercept therapy. During her physical exam, you notice her spleen is 4 cm below the costal margin, and she has bilateral swelling of the MCP joints; otherwise all other findings are normal. Her CBC is as follows:
| WBC | 8900/µL |
| Absolute Neutrophil Count | 451/µL |
| Absolute Lymphocyte Count | 7900/µL |
| Hgb | 10.5 g/dl |
| MCV | 89 fL |
| PLT | 325k/µL |
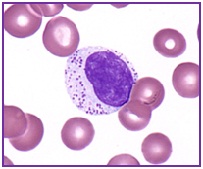
You review her peripheral smear and more than 60 percent of WBCs are similar to the cell seen in the image on the left.
Flow cytometry of the peripheral blood shows CD3+ CD4- CD8+ CD57+ TCRαβ+immunophenotype of the lymphocytes. TCR-γ gene rearrangement is detected in the peripheral blood by PCR.
What is the best course of treatment?
- Observation
- "7+3" chemotherapy
- Lenalidomide 10 mg per day
- Methotrexate 10 mg/m2 per week
- 1 gram of methylprednisolone sodium succinate daily for 3 days
Answer
- Methotrexate 10 mg/m2 per week
Explanation
Large granular lymphocyte (LGL) leukemia is a clonal disorder of cytotoxic CD3+CD8+ T cells (T-LGL) or CD3-CD8+ natural killer cells (NK-LGL). T-LGL leukemia is associated with rheumatoid arthritis (RA) in 11 to 36 percent of cases.1 It is less commonly associated with other autoimmune conditions such as systemic lupus erythematous and Sjögren syndrome. Patients with T-LGL may present with clinical manifestations such as anemia, neutropenia, lymphocytosis, and splenomegaly.
Normally, LGLs can be found in the peripheral blood at low numbers (up to 0.25 x 109/L). LGLs are large in size (15-18 µm) and have abundant cytoplasm with azurophilic granules. Diagnosis is made when there is an increase in the number of circulating LGLs and clonality can be detected by TCR-γ gene rearrangement. Polyclonal expansion of LGLs is seen in many conditions including HIV, after solid organ or bone marrow transplants, and post-splenectomy.2
For asymptomatic patients with T-LGL leukemia, observation may be an option. Although large clinical trials are needed to confirm, experts suggest treating patients who have 1) severe neutropenia defined as an ANC less than 500; 2) moderate neutropenia (ANC 500 -1,500) with recurrent infections; 3) symptomatic or transfusion-dependent anemia; and 4) an associated, symptomatic, autoimmune disease.1,3
First-line treatment for patients with T-LGL leukemia usually consists of immunosuppressive agents such as methotrexate 10 mg/m2 per week +/- prednisone, with overall response rates in the largest trial of 62 patients being 55 percent.4 Responses should be evaluated after four months of treatment so that potentially effective treatments are not abandoned prematurely. For those patients who do not respond to methotrexate, cyclosporine A or oral cyclophosphamide (100 mg/day) are reasonable second-line options.
Resources
- Lamy T, Loughran TP Jr. How I treat LGL leukemia. Blood. 2011;117:2764-2774.
- Rose MG, Berliner N. T-cell large granular lymphocyte leukemia and related disorders. Oncologist. 2004;9:247-258.
- Zhang D, Loughran TP Jr. Large granular lymphocytic leukemia: molecular pathogenesis, clinical manifestations, and treatment. ASH Education Program. 2012;2012:652-659.
- Bareau B, Rey J, Hamidou M, et al. Analysis of a French cohort of patients with large granular lymphocyte leukemia: a report on 229 cases. Haematologica. 2010;95:1534-1541.
- Venroij, WJ et al. Anti-CCP antibodies: the past, the present and the future. Nat Rev Rheumatol. 2011;7:391-398.