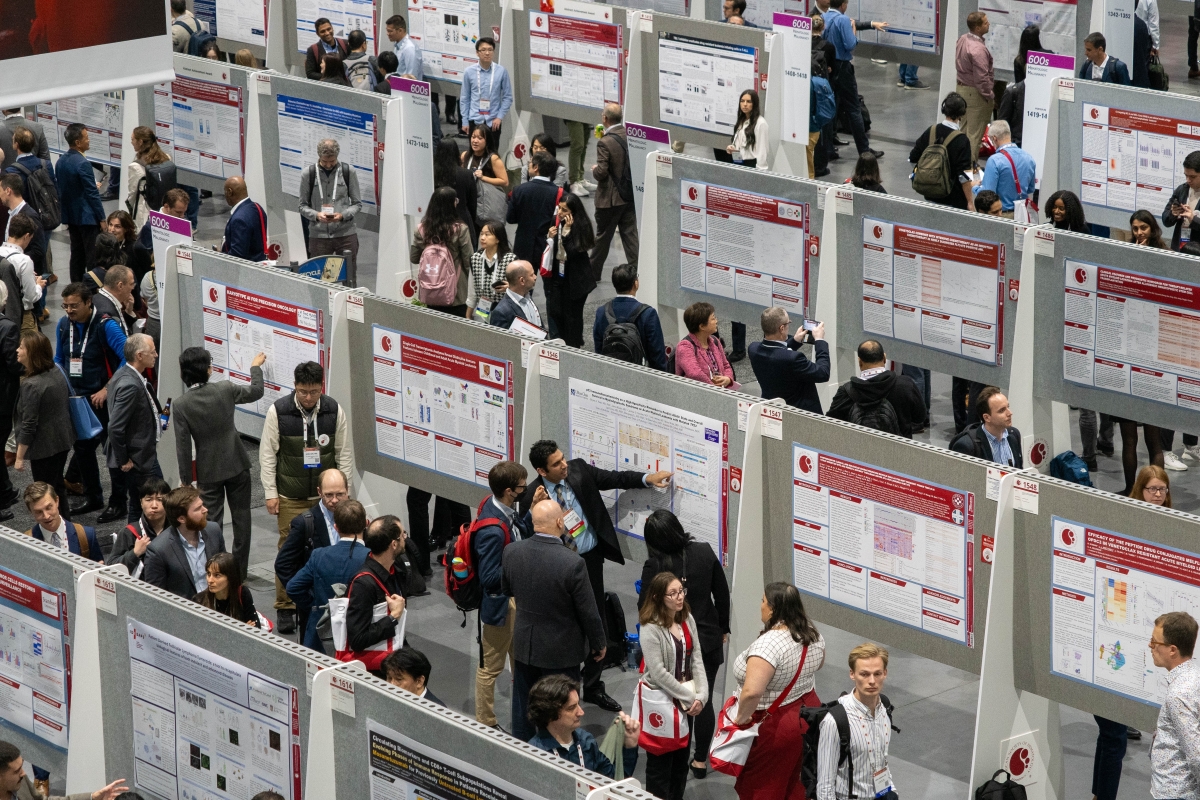
With more than 18,000 members from nearly 100 countries, ASH is the world's largest professional society serving both clinicians and scientists around the world who are working to conquer blood diseases.

Commitment to Excellence Through Expansion and Inclusion
As the world’s largest professional society of clinicians and scientists dedicated to conquering blood diseases, ASH seeks to expand the availability of hematologic care while promoting the highest standards of excellence in hematology research, training, and practice.
Commitment to Transformative Research
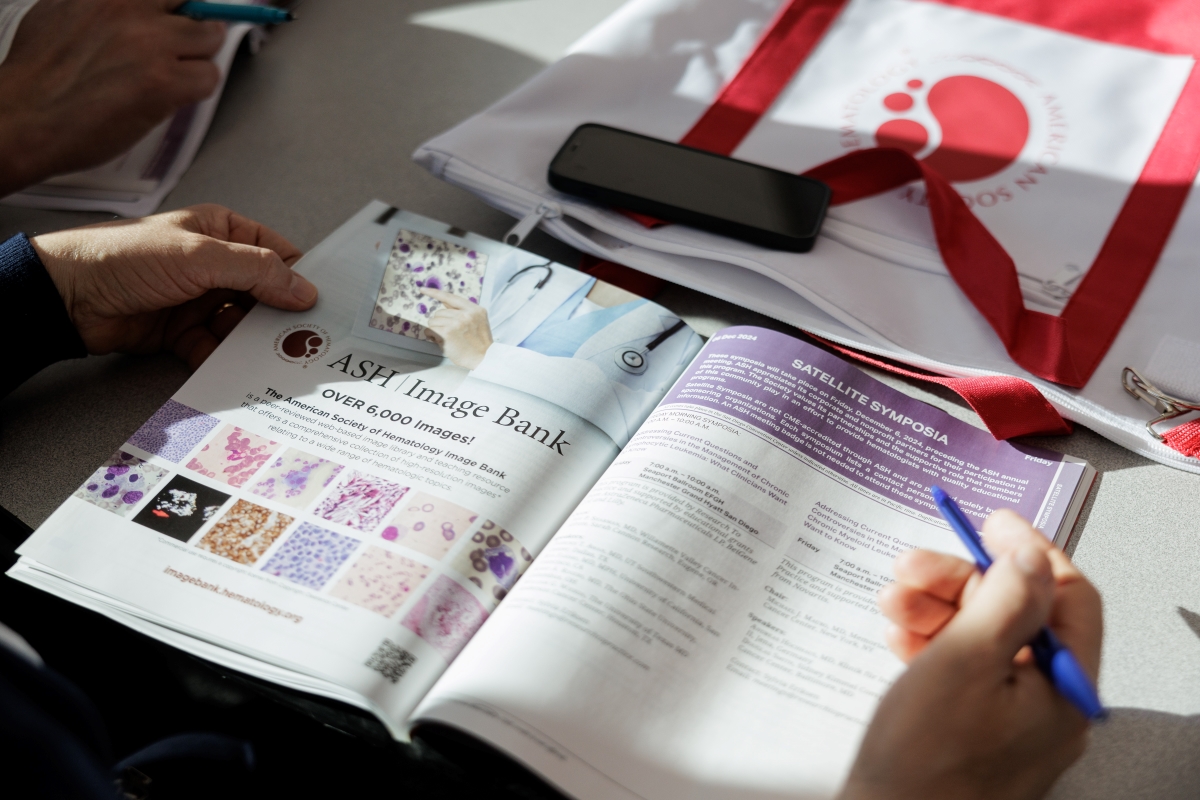
ASH leads the world in promoting and supporting clinical and scientific hematology research through its many innovative award programs, meetings, publications, and advocacy efforts.
Commitment to Innovative Hematology Education and Training
ASH is the world's leading provider of hematology education and offers a wide array of educational resources and services for clinicians and scientists at any stage in their careers.
Who We Are
With more than 18,000 members from nearly 100 countries, ASH is the world's largest professional society serving both clinicians and scientists around the world who are working to conquer blood diseases.
History of ASH
In April 1958, the first official meeting of the American Society of Hematology was held in Atlantic City, New Jersey, where more than 300 hematologists gathered to discuss clinical and research matters related to blood and blood diseases. Since that initial meeting, ASH has played an active and important role in the development of hematology as a discipline.
Structure and Governance
The Society is governed by its Executive Committee composed of the president, president-elect, vice president, secretary, treasurer, and eight councilors, all of whom are elected by Society members. The Society has 14 standing committees, which recommend policies, programs, and actions to the Executive Committee.
Get Involved
ASH supports hematologists in their mission to conquer blood diseases, relying on the leadership, guidance, and hard work of numerous volunteers. Explore ways you can lend your time, expertise, and generosity.









