Research Exposes Inequities in Health Care Access and Delivery for Blood Disorders
Scientists identify barriers and suggest opportunities to close gaps
(NEW ORLEANS, La., Dec. 10, 2022) – Four studies presented during the 64th American Society of Hematology (ASH) Annual Meeting and Exposition uncover significant disparities in medical care and health outcomes among patients of different racial backgrounds, nationalities, and socioeconomic status across a range of blood disorders. The new findings underscore the importance of acting intentionally to close gaps in the health care system and ensure care is delivered equitably.
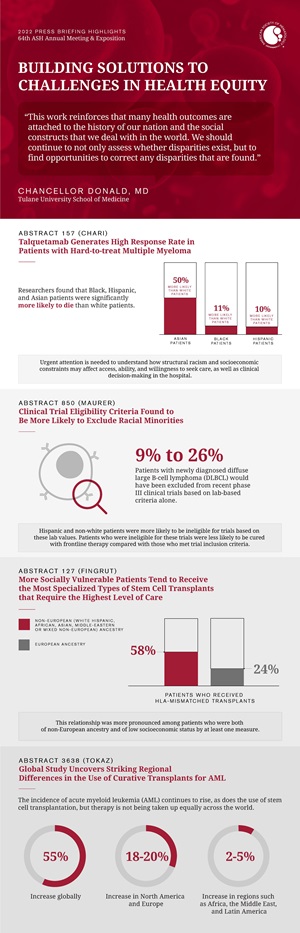 “This work reinforces that many health outcomes are attached to the history of our nation and the social constructs that we deal with in the world,” said press briefing moderator Chancellor Donald, MD, of Tulane University School of Medicine. “We consistently find that there’s work to be done, and researchers should continue not only to assess whether disparities exist, but to find opportunities to correct any disparities that they find.”
“This work reinforces that many health outcomes are attached to the history of our nation and the social constructs that we deal with in the world,” said press briefing moderator Chancellor Donald, MD, of Tulane University School of Medicine. “We consistently find that there’s work to be done, and researchers should continue not only to assess whether disparities exist, but to find opportunities to correct any disparities that they find.”
Dr. Donald added that proactively working to address disparities can go a long way toward achieving better outcomes even without new tests or therapies. For instance, one study found stark differences in the types of therapies used to treat pulmonary embolism in different groups along with disparities in associated death rates, suggesting an opportunity for clinicians to employ existing tools more effectively across all groups.
A second study focuses on the importance of diverse representation in clinical trials. The third and fourth studies highlight inequities in the delivery of stem cell transplants in the United States and globally, pointing to opportunities to improve access to this potentially curative treatment.
The press briefing aired on the annual meeting virtual platform on Wednesday, December 7, at 1:00 p.m. Central time.
Stark Social Disparities Seen in Treatments and Outcomes for Pulmonary Embolism
140: Social Determinants of Health and Pulmonary Embolism Treatment and Mortality: The Nationwide Inpatient Sample
Racial minorities and people with lower incomes or who are insured by Medicare or Medicaid are significantly less likely to receive the most advanced therapies and more likely to die after suffering a pulmonary embolism (PE), according to a new analysis. A PE occurs when a blood clot blocks an artery in the lung, typically leading to chest pain and shortness of breath. It is a medical emergency that without timely treatment – medications or procedures to remove the clot – can cause death.
The study, based on data from more than 1 million patients in the United States, found that 6.4% of those hospitalized for PE died of the condition, a strikingly high case-fatality rate that further underscores the urgency of reducing disparities and improving access to care, according to researchers.
“In order to solve the disparities we see, we need to shine a light on them,” said Mary Cushman, MD, MSc, of the Larner College of Medicine at the University of Vermont. “Many people die of pulmonary embolism every year. It’s preventable and it’s certainly treatable. We need to think about what we can do in hospitals to make sure that care is equitable.”
The researchers analyzed records from more than 1.1 million people hospitalized with PE from 2016-2018, including about 66,000 with the most severe form of PE. They first analyzed which patients received advanced therapies, such as the use of a heart-lung machine or treatments in which doctors use a catheter or surgical intervention to break up the clot. They then assessed rates of in-hospital death from PE. For both analyses, researchers adjusted for hospital type, age, sex, and other risk factors to assess the influence of race, income, or insurance type independent of other factors.
Among people with the most severe PE, researchers found that Black, Hispanic, and Asian patients were significantly more likely to die than white patients. Among all racial groups, the overall rate of PE was lowest among Asian people, but Asian patients were 24% less likely to receive advanced therapies and 50% more likely to die compared with white patients. Black patients with high-risk PE were 13% less likely to receive advanced therapies compared with white patients, and 11% more likely to die. Hispanic patients were 10% more likely to die than white patients. People insured by Medicare or Medicaid were around 30% less likely to receive advanced therapies than privately insured people, and people in the lowest quartile for income were 9% more likely to die than people in the highest quartile for income.
Researchers say urgent attention is needed to better understand how factors such as structural racism and socioeconomic constraints may affect a person’s access, ability, and willingness to seek care, as well as clinical decision-making once patients arrive at the hospital.
“I hope that clinicians will think about these findings in terms of how they take care of patients every day, and try their best to recognize their unconscious biases,” said Dr. Cushman. “Clinicians need to look at the patient in front of them and remember that regardless of their social class or the color of their skin, they should be treated the same as everybody else.”
Mary Cushman, Larner College of Medicine at the University of Vermont, will present this study during an oral presentation on Saturday, December 10, 2022, at 12:15 p.m. Central time in Great Hall B/C.
Clinical Trial Eligibility Criteria Found to Be More Likely to Exclude Racial Minorities
850: Evaluating the Impact of Lab-Based Eligibility Criteria by Race/Ethnicity in Frontline Clinical Trials for Diffuse Large B-Cell Lymphoma (DLBCL): A LEO Cohort Analysis
People with diffuse large B-cell lymphoma (DLBCL) were much less likely to be eligible to participate in clinical trials to test new frontline therapies for the disease if they were in a minority racial or ethnic group, according to a new study. Even though the clinical trials examined in the study do not exclude patients based on race or ethnicity directly, the results show that patients in minority groups were more likely to fall short of trial criteria based on levels of hemoglobin, neutrophil count, platelet count, creatinine, and bilirubin – laboratory tests commonly used to determine trial eligibility.
“Our research has shown that about a quarter of patients are being excluded from frontline trials based on these five criteria alone,” said Matthew Maurer, DMSc, of Mayo Clinic in Rochester, Minnesota. “These are patients who want to participate in research have the resources to go to an academic medical center, and yet these exclusion criteria are not impacting everyone equally – they’re impacting minorities more than white non-Hispanic patients.”
DLBCL is an aggressive lymphoma and the most common type of lymphoma in the United States. While standard upfront therapies are curative for about 60% of patients, researchers have struggled to find effective agents for treating the remaining patients.
Laboratory values are typically included in eligibility criteria for clinical trials to ensure participants are healthy enough to complete their assigned standard or experimental treatment course. At the same time, researchers seek to enroll a diverse group of participants to ensure the population of trial participants reflects the patient population affected by that disease.
The study is based on data from the Lymphoma Epidemiology Outcomes (LEO) Cohort, an observational cohort study that prospectively enrolls and follows patients with lymphoma from eight large academic medical centers across the United States. Researchers analyzed health records from 2,185 patients in LEO to assess which patients would satisfy the eligibility criteria for eight recent DLBCL clinical trials. About 76% of those included in the sample were non-Hispanic white and 24% were Hispanic and/or non-white.
Overall, the researchers found that 9 to 26% of LEO Cohort patients with newly diagnosed DLBCL would have been excluded from recent phase III clinical trials based on lab-based criteria alone. These lab values varied significantly by race and ethnicity. As a result, Hispanic and non-white patients were more likely to be ineligible for trials based on these lab values. Patients who were ineligible for these trials were less likely to be cured with frontline therapy compared with those who met trial inclusion criteria.
To ensure the broadest possible group of patients can benefit from clinical trial participation – and ultimately benefit from therapies that have been well-tested in diverse populations – researchers say further study is needed to determine which lab-based eligibility criteria are most meaningful to inform future trial designs.
“We know that how we design clinical trials and how we set their eligibility criteria impacts patient enrollment,” said Dr. Maurer. “We need to be more inclusive in the clinical trials that we do, in particular, to be more inclusive of Hispanic and non-white populations.”
Matthew Maurer, Mayo Clinic, will present this study during an oral presentation on Monday, December 12, 2022, at 3:30 p.m. Central time in La Nouvelle Orleans Ballroom C.
More Socially Vulnerable Patients Tend to Receive the Most Specialized Types of Stem Cell Transplants that Require the Highest Level of Care
127: Analysis of 372 Adult Allograft Recipients Reveals Associations between Non-European Ancestry, Low Socioeconomic Status, and Receipt of HLA-Disparate Grafts
People of non-European ancestry and especially those of low socioeconomic status are more likely to receive the most specialized types of allogeneic stem cell transplantation which require the highest level of care, according to a new study.
Allogeneic stem cell transplantation is a potentially curative treatment for people with life-threatening blood cancers, but this procedure requires an allograft (tissue donation) from a suitable donor. Doctors aim to find a donor with the same human leukocyte antigen (HLA) proteins as the patient to minimize the risk of a dangerous immune reaction. If an HLA-identical donor is not available in the family, doctors usually prefer an HLA-matched volunteer unrelated donor, if available. For patients without these options, doctors can perform a more specialized type of transplant using stem cells from HLA-mismatched cord blood, half-matched family members, or HLA-mismatched unrelated donors.
This new study co-led by Warren Fingrut, MD, of the Cord Blood Transplantation Program at Memorial Sloan Kettering Cancer Center (MSK) in New York, is the first to investigate how interactions between racial background and socioeconomic status relate to the types of allografts patients receive. While previous studies have shown that patients of non-European ancestry are less likely to receive a transplant from a matched unrelated donor, these new findings reveal that the interaction between racial background and socioeconomic status, not just race/ethnicity alone, is an important factor. The study also revealed discrepancies in the metrics used to assess socioeconomic status, underscoring the need for better data.
“Our transplant program is very committed to extending transplant access to minority populations, but our study highlights that many of these patients are both receiving the most complex transplants and facing significant socioeconomic challenges,” said Dr. Fingrut. “Our findings show that addressing financial hardship will be critical to extend transplant access, especially to patients from minority groups.”
The researchers analyzed health records from 372 people who underwent allogeneic transplantation at MSK between 2020-2022. About 70% had European ancestry and the rest had white Hispanic, African, Asian, Middle-Eastern, or mixed non-European ancestry. Since household income data were not available, researchers assessed patients’ socioeconomic status using four surrogate metrics: Medicaid insurance, area deprivation index (which reflects a neighborhood’s poverty level), whether the patient received financial support for cost-of-living (for housing, food, or transportation), and medical expenses.
Overall, 58% of patients with non-European ancestry received HLA-mismatched transplants, compared with 24% among those with European ancestry. This relationship was more pronounced among patients who were both of non-European ancestry and of low socioeconomic status by at least one measure. However, different metrics resulted in different patients being classified as having low socioeconomic status, suggesting that no single surrogate metric perfectly captures all patients who may be facing economic hardship. To better understand these nuances, researchers said medical centers should proactively collect data on patients’ income and employ a mix of methods to assess patients’ socioeconomic status.
“In order to address disparities, we must describe them, understand them, and delve into their causes,” said Dr. Fingrut. “It’s not just the highly specialized medical care that’s needed for these more vulnerable patients – our study also speaks to the resources needed to support them.”
Warren Fingrut, Memorial Sloan Kettering Cancer Center, will present this study during an oral presentation on Saturday, December 10, 2022, at 9:30 a.m. Central time in 388-390.
Global Study Uncovers Striking Regional Differences in the Use of Curative Transplants for AML
3638: An Analysis of the Worldwide Utilization of Hematopoietic Stem Cell Transplantation for Acute Myeloid Leukemia
The use of stem cell transplantation for acute myeloid leukemia (AML) increased by about 55% worldwide between 2009-2016, according to a new study. Although the largest increases were seen in lower- and middle-income countries, patients in these countries still face the greatest barriers when it comes to accessing this important therapy, researchers said. Allogeneic stem cell transplants (which use stem cells from a donor and are the only curative therapy for the majority of patients with AML) accounted for the vast majority of the increase in stem cell transplantation overall, while rates of autologous transplants (which use a patient’s own stem cells and are used as an augment to allow for more intensive use of chemotherapy) declined significantly.
“The incidence of AML continues to rise, as does the use of stem cell transplantation, but this therapy is not being taken up equally across the world,” said Molly Tokaz, MD, of the University of Washington. “Utilization rates are lagging in lower resourced regions, and we’ve got a lot of ground to cover to get utilization where we want it. Since an allogeneic transplant is a curative treatment, this difference in uptake has profound implications for what kinds of outcomes we can expect for these patients.”
The study is based on data from the Global Burden of Disease project and Worldwide Network for Blood and Marrow Transplantation. Researchers found that AML rates rose by about 2,000 diagnoses per year over the study period, reflecting an overall uptick in AML incidence globally with about 118,000 new diagnoses in 2016. The rate of stem cell transplantation increased by 55% overall from 2009 to 2016, but the use of transplantation as a percentage of patients with AML remained relatively low in many countries.
Even in well-resourced regions like North America and Europe, only about 18 to 20% of AML patients of all ages received a stem cell transplant in 2016. While this is much higher than the 2 to 5% seen in regions such as Africa, the Middle East, and Latin America, it suggests there is still room for improvement in all regions of the world, researchers said. The researchers also noted that more allografts were from unrelated donors in higher income countries compared with lower income countries, where donors were most often related to the recipient. These differences likely reflect the complex infrastructure required to match patients and facilitate transplants with unrelated donors.
Although the study only used data through 2016, other ongoing studies suggest the reported trends have continued in the intervening years, with many countries seeing an increase in the use of stem cell transplantation but significant gaps remaining between resource-rich and resource-poor regions, researchers noted.
Dietger Niederweiser, University of Leipzig, will present this study during an oral presentation on Sunday, December 11, 2022, at 6:00 p.m. Central time in Hall D.
Additional press briefings will take place throughout the meeting on pediatric cancer care, advances in blood cancer research and care, novel drug development, and selected late-breaking abstracts. For the complete annual meeting program and abstracts visit www.hematology.org/annual-meeting. Follow ASH and #ASH22 on Twitter, Instagram, LinkedIn, and Facebook for the most up-to-date information about the 2022 ASH Annual Meeting.
The American Society of Hematology (ASH) (www.hematology.org) is the world’s largest professional society of hematologists dedicated to furthering the understanding, diagnosis, treatment, and prevention of disorders affecting the blood. For more than 60 years, the Society has led the development of hematology as a discipline by promoting research, patient care, education, training, and advocacy in hematology. ASH’s flagship journal, Blood (www.bloodjournal.org), is the most cited peer-reviewed publication in the field, and Blood Advances (www.bloodadvances.org), is the Society’s online, peer-reviewed open-access journal.
Contacts:
Leah Enser, ASH, [email protected]
Kira Sampson, ASH, [email protected]
Brianne Cannon, FleishmanHillard, [email protected]