CAR T-cell Therapy Found Equivalent to Standard of Care as Second-line Treatment for Aggressive non-Hodgkin Lymphoma
Study in ASH Late-Breaking Abstracts session gives new insights into the administration of CAR T-cell therapy
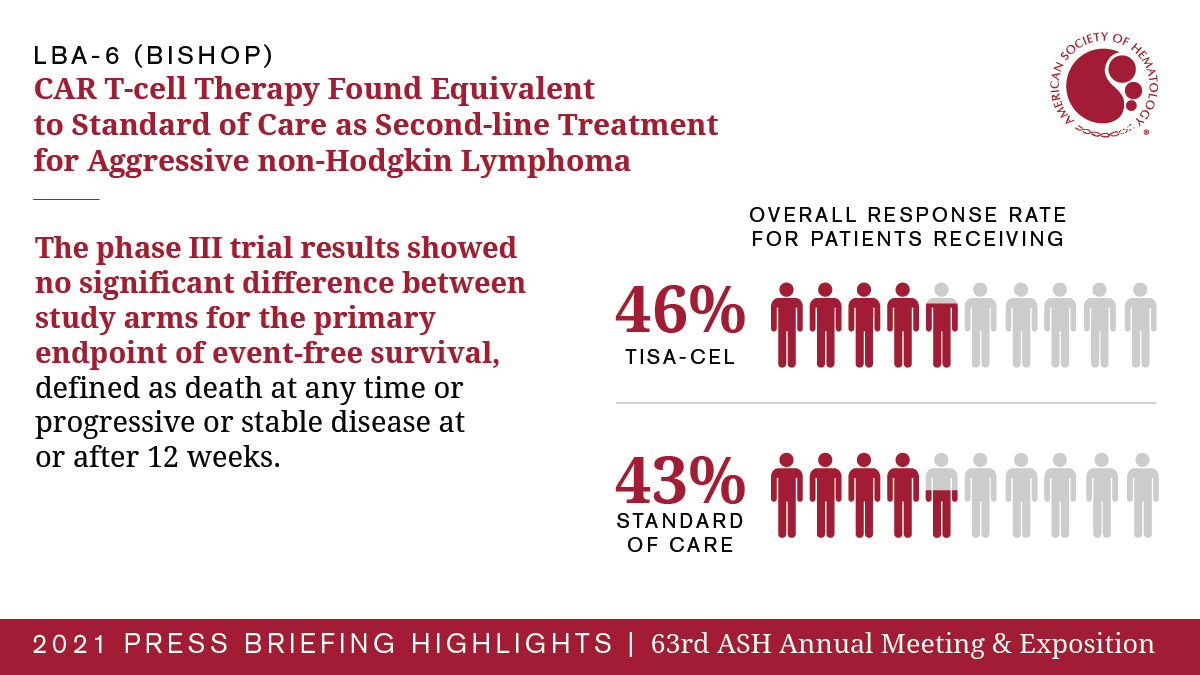
(WASHINGTON, Dec. 14, 2021) – In a phase III trial presented during the 63rd American Society of Hematology (ASH) Annual Meeting and Exposition, the chimeric antigen receptor (CAR) T-cell therapy tisagenlecleucel (tisa-cel) was not found to improve event-free survival over what was seen with standard of care as a second-line treatment for patients with aggressive non-Hodgkin lymphoma. The results, which come as a surprise after previous CAR-T trials have shown improved clinical outcomes, may reflect variability in the patient population, timing and administration of tisa-cel and stem cell transplants, and use of chemotherapy in real-world settings, according to researchers.
In CAR T-cell therapies, a patient’s T cells are removed and a gene for a receptor that binds a specific protein on cancer cells is added to help them find and destroy cancer cells. Then, the modified cells are infused back into the patient. Tisa-cel has previously been found beneficial as a third-line treatment for patients with aggressive non-Hodgkin lymphoma who typically have an extremely poor prognosis. The new study sought to determine whether tisa-cel could offer benefits earlier in the course of treatment as a second-line therapy before attempting a stem cell transplant.
“We were surprised that event-free survival was identical in both study arms,” said Michael R. Bishop, MD, of The David and Etta Jonas Center for Cellular Therapy, University of Chicago. “This suggests there is still a lot to be learned about the proper administration of CAR-T therapies. As this field progresses, we’re learning that there may be more variables to consider as we seek to optimize CAR-T therapies.”
The trial enrolled 322 patients with aggressive B-cell non-Hodgkin lymphoma who did not respond to initial chemotherapy or relapsed within 12 months. Patients were randomly assigned to receive tisa-cel or standard of care, which consisted of chemotherapy followed by an autologous stem cell transplant for patients responding to chemotherapy. The majority of patients randomized to receive tisa-cel also received chemotherapy before their CAR T-cell therapy, a treatment strategy known as “bridging,” at their physician’s discretion. At the time of reporting, researchers had tracked patient outcomes for a median of 10 months.
The results showed no significant difference between study arms for the primary endpoint of event-free survival, defined as death at any time or progressive or stable disease at or after 12 weeks. Twenty-eight percent of patients in both study arms showed a complete response to treatment, and the overall response rate was also similar (46% in those receiving tisa-cel versus 43% in those receiving standard of care).
Researchers identified several factors that may have potentially contributed to the current results. As an international trial conducted in 18 countries, researchers observed some real-world variability in the treatment strategies used in different regions and countries. Use of bridging therapy was not uniform, and this led to more patients with progressive disease at infusion, which was associated with a worse outcome. In particular, patients treated in non-U.S. centers tended to receive more cycles of bridging chemotherapy. Time to infusion was also quite variable; overall, patients waited a median of 52 days for their CAR-T infusion after leukapheresis (the first step in CAR T-cell therapy), which is relatively long given the aggressive nature of the disease. Time to infusion was shorter in the U.S. compared with non-U.S. countries. In addition, patients in the standard of care arm were allowed to receive up to two different regimens before the strategy was considered a failure. Researchers also noted some potentially meaningful differences between the treatment arms in specific patient groups in terms of disease biology and prognostic factors, and they plan to further analyze the data to understand how these factors may have played a role in the results.
“These findings show the importance of doing randomized trials and comparing their results to help improve outcomes for patients,” said Dr. Bishop. “It gives us tremendous insights into the biology of these very aggressive diseases and points to an opportunity to more closely examine many factors, in particular the role and timing of bridging therapy.”
About half of patients randomized to receive standard of care crossed over to receive tisa-cel, with outcomes similar to those found in previous trials of tisa-cel as a third-line therapy in the same patient population. Both patient groups experienced a relatively high rate of adverse events, but the overall safety profile was consistent with previous studies in this patient population. Fatal adverse events occurred in 10 patients who received tisa-cel and 13 who received standard of care.
The investigators are now performing additional analyses to determine factors that may have affected outcomes in both treatment arms.
The study was funded by Novartis Pharmaceuticals Corporation.
Michael R. Bishop, MD, David and Etta Jonas Center for Cellular Therapy, University of Chicago, will present this study during an oral presentation on Tuesday, December 14, at 9:00 a.m. Eastern time in Hall C2-C3.
Press Briefing Highlights
Additional press briefings took place throughout the meeting on immunotherapy, new insights into blood disorders, COVID-19, and diversifying care in acute leukemia. For the complete annual meeting program and abstracts, visit www.hematology.org/annual-meeting. Follow ASH and #ASH21 on Twitter, Instagram, LinkedIn, and Facebook for the most up-to-date information about the 2021 ASH Annual Meeting.
The American Society of Hematology (ASH) (www.hematology.org) is the world’s largest professional society of hematologists dedicated to furthering the understanding, diagnosis, treatment, and prevention of disorders affecting the blood. For more than 60 years, the Society has led the development of hematology as a discipline by promoting research, patient care, education, training, and advocacy in hematology. ASH publishes Blood (www.bloodjournal.org), the most cited peer-reviewed publication in the field, and Blood Advances (www.bloodadvances.org), an online, peer-reviewed open-access journal.
Contact:
Leah Enser, American Society of Hematology
[email protected], 202-552-4927