Studies Shed Light on New Treatment Approaches, Future Targets for Clot Busting
(Orlando, FL, Dec. 7, 2019) — Three studies being presented today during the 61st American Society of Hematology (ASH) Annual Meeting and Exposition in Orlando help advance the treatment of adult and pediatric patients at risk of developing venous thromboembolism (VTE), the formation of blood clots in the veins that can lead to heart attack, stroke or pulmonary embolism, disability, and death.
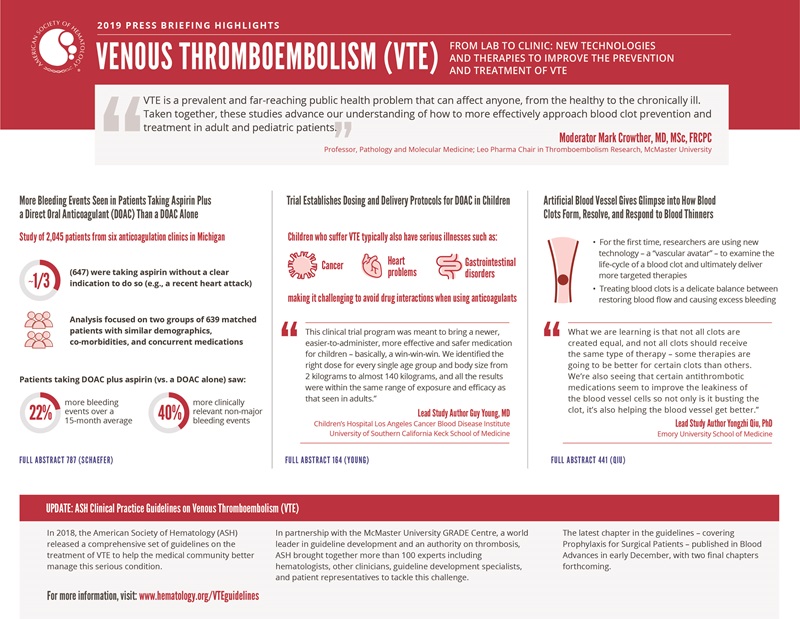
The first study, which included people with atrial fibrillation – an irregular heart rhythm – or a history of VTE, found that taking an aspirin in addition to a direct oral anticoagulant (DOAC) led to more bleeding episodes, but similar rates of stroke, VTE, and heart attacks compared with taking a DOAC alone.
“Many people are on several anticoagulants and blood thinners simultaneously, but we are seeing a big shift in medicine to embrace ‘less is more,’” said press briefing moderator, Mark Crowther, MD, of McMaster University, Ontario, Canada. “This study adds to our understanding and underscores the need to actively review what patients are taking and what ideally is needed to both reduce the risk of blood clots and minimize bleeding.”
For children who develop blood clots, a phase III study established, for the first time, an easy-to-administer liquid formulation and dosing regimen for the DOAC, rivaroxaban. Dr. Crowther added that, while rivaroxaban is not yet approved for pediatric use, the data confirm it can be used safely and effectively in children and the oral formulation will likely be much preferred to daily injections, which have been the standard of care.
In a third study, researchers used cutting-edge technology to develop an artificial blood vessel to examine how blood clots form and resolve over time either naturally or in response to various anticoagulant medications. Researchers say the study is yielding useful insights that can help inform future studies and ultimately inform clinical practice aimed at reducing VTE. “Ultimately, these innovations may reduce the need for experiments in animals and may make studies in humans easier as they will allow greater insights into drug behavior before they are used in humans.” Dr. Crowther said.
“Taken together, these studies advance our understanding of how to more effectively approach blood clot prevention and treatment in adult and pediatric patients.” Dr. Crowther said.
ASH recently released a comprehensive series of clinical practice guidelines on VTE to help the medical community better manage this serious condition. The most recent guideline was published this week and focuses on prevention of VTE in surgical patients. ASH plans to release additional VTE guidelines in 2020.
This press conference will take place on Saturday, December 7, at 9:30 a.m. in the ASH press briefing room W221DE.
More Bleeding Events Seen in Patients Taking Aspirin Plus a DOAC Than a DOAC Alone
#787 Impact of Adding Aspirin to Direct Oral Anticoagulant Therapy without an Apparent Indication
Patients with atrial fibrillation or a history of VTE who take a daily aspirin in addition to a prescribed DOAC to treat or prevent blood clots had significantly higher rates of bleeding complications compared with those taking a DOAC alone, according to a new report from six anticoagulation clinics across the state of Michigan. Researchers also found no differences in stroke, heart attack, or blood clots between the groups after one year.
“The role of aspirin in combination with the newer DOACs is not well understood,” said lead study author Jordan Schaefer, MD, of the Division of Hematology/Oncology at the University of Michigan. “Based on our findings, adding aspirin may do more harm than good for some patients, increasing bleeding rates without improvements in the incidence of thrombosis.”
Of the 2,045 patients initially followed for the study, nearly one-third (647) were taking aspirin even though there was no clear indication to do so, such as a recent heart attack.
“We continue to see high numbers of patients taking aspirin, which is readily available over-the-counter, and that means clinicians may not know a patient is taking it,” Dr. Schaefer said. “There must be careful consideration of the relative risks and benefits of adding or continuing aspirin for patients on DOAC therapy.”
DOACs such as apixaban, dabigatran, edoxaban, and rivaroxaban are a newer group of blood thinners that are frequently prescribed to prevent stroke in people with atrial fibrillation, a common and serious heart rhythm disorder, and treat or guard against repeat episodes of deep vein thrombosis or pulmonary embolism. Records did not indicate whether aspirin therapy was initiated by the patient or recommended by a clinician.
Of the total number of patients, researchers focused their analysis on two groups of 639 matched patients that had similar demographics, co-morbidities, and concurrent medications. Of the patients taking aspirin, most (90.3%) were taking low dose aspirin (≤ 100 mg per day). Compared with patients taking a DOAC alone, those taking a DOAC plus aspirin had 319 versus 261 bleeding events, a 22% jump in bleeds, over an average follow-up of 15 months. This difference was largely driven by clinically relevant non-major bleeding events, which were nearly 40% higher with dual therapy. Bleeding sites were most commonly bruising, intestinal bleeding, or bleeding through the urinary tract. Observed rates of thrombosis (stroke, VTE, and heart attacks) were similar between patients taking both medicines and those only on a DOAC (19 and 18 events). The only two fatal bleeding events were seen among patients on DOACs only. Patients on combination therapy had more emergency room visits and hospitalizations mostly due to bleeding, but these differences did not reach statistical significance.
“For patients prescribed a DOAC, whether to add or continue aspirin is a common clinical question. For some patients, we didn’t see a clear benefit,” Dr. Schaefer said. “It’s really important for clinicians to assess whether patients are using aspirin and, equally, it’s important that patients not simply take a medicine because it’s easy to get over-the-counter, but rather talk with their doctor about whether it’s safe and whether there is an important need for it.”
He said he hopes these data will raise awareness within the medical community and lead to interventions aimed at reducing the number of patients inappropriately on aspirin perhaps by instituting electronic medical record alerts or leveraging local anticoagulation experts.
The current study further bolsters earlier research by Dr. Schaefer and his team published in JAMA Internal Medicine that found that some patients using aspirin and warfarin, a different type of anticoagulant, experienced a higher rate of bleeding events compared with those taking warfarin alone. Similar to the current study, there were no observed difference in rates of heart attack, stroke, or VTE. Further study is needed to determine whether DOACs plus aspirin is safer than warfarin plus aspirin and to be able to compare bleeding events and the outcomes of the individual DOACs.
Although the study is limited to Michigan, researchers said the mix of clinics were representative of different patients, geographic regions (urban, suburban, and rural), and academic and community centers. Because of the small size of the study, the researchers caution that they were not able to fully assess for differences in clotting outcomes or evaluate some important subgroups, including those that might benefit from adding aspirin.
Jordan K. Schaefer, MD, University of Michigan will present this study during an oral presentation on Monday, December 9, at 2:45 p.m. in Valencia BC (W415BC).
Trial Establishes Dosing and Delivery Protocols for Direct Oral Anticoagulant in Children
#164 Rivaroxaban for Treatment of Pediatric Venous Thromboembolism an Einstein-Jr Phase III Dose-Exposure-Response Evaluation
A phase III clinical trial confirms that children with dangerous blood clots known as VTE can be safely and effectively treated with the direct oral anticoagulant rivaroxaban using formulations and dosing regimens that are tailored for children from birth to age 17.
While direct oral anticoagulants have been approved for treating adults for nearly a decade, the trial is the first to develop a liquid formulation suitable for use in young children.
“This clinical trial program was meant to bring a newer, easier-to-administer, more effective, and safer medication for children – basically, a win-win-win,” said lead study author Guy Young, MD, of the Children’s Hospital Los Angeles Cancer and Blood Disease Institute and the University of Southern California Keck School of Medicine. “We identified the right dose for every single age group and body size from 2 kilograms to almost 140 kilograms, and all the results were within the same range of exposure and efficacy as that seen in adults.”
The trial reported safety and efficacy results in mid-2019, finding that children treated with rivaroxaban had similar rates of recurrent VTE and clinically relevant bleeding as those receiving standard pediatric anticoagulation therapy. The new results shed light on the appropriate dose, schedule, and formulation for administering rivaroxaban to children of various ages and body sizes.
Expanding the use of a drug from adults to children is complicated. One reason is the enormous differential in body size between a newborn baby and an adult-sized teen. In addition, children metabolize drugs differently than adults, which can necessitate giving two to three smaller doses over the course of a day rather than a single larger dose. For drugs like rivaroxaban that were originally developed as a tablet, it is also necessary to create a liquid formulation for young children.
The trial was conducted from 2014-2018 and administered rivaroxaban to 365 children from birth to 17 years old. About 38% of participants received rivaroxaban in tablet form and 62% received the liquid formulation. Participants received the drug once, twice, or three times daily.
The study’s dosing protocols were found to result in a similar level of exposure and similar outcomes in terms of efficacy, bleeding, and adverse events compared to adults receiving a 20 mg tablet of rivaroxaban daily. Imaging results indicated VTE was stabilized or improved in about 80% of children taking rivaroxaban, while just 0.6% experienced symptomatic recurrent VTE. The liquid formulation was also found to be acceptable and palatable.
Children who suffer VTE typically have serious illnesses such as cancer, heart problems, or gastrointestinal disorders, making it challenging to avoid drug interactions when using anticoagulants. Standard options such as coumadin and heparin can be difficult to use alongside other drugs and often require frequent injections and laboratory monitoring. Direct oral anticoagulants are advantageous because they have few drug interactions and are simple to administer, Dr. Young said.
Guy Young, MD, of the Children’s Hospital Los Angeles Cancer and Blood Disease Institute and the University of Southern California Keck School of Medicine, will present this study during an oral presentation on Saturday, December 7, at 12 noon in W314.
Artificial Blood Vessel Gives Glimpse into How Blood Clots Form, Resolve, and Respond to Blood Thinners
#441 Monitoring the “Lifetime” of a Thrombus over Long Timescales by Leveraging a Novel Microvasculature-on-Chip Thrombosis Resolution Assay
New technology is allowing researchers at the Emory University School of Medicine to grow blood clots in a controlled environment and examine the life-cycle of thrombosis that commonly leads to heart attack, stroke, pulmonary embolism, and other life-threatening events, to ultimately better target therapies. Researchers are using a novel assay, which they have dubbed a “vascular avatar” as a stand-in for an actual blood vessel to gather fundamental knowledge about how a thrombosis resolves and to test how different drugs or a cocktail of drugs might accelerate the process.
“The way we typically treat blood clots is to give medicines that cause someone to bleed to restore blood flow and avoid ischemic injury, but we don’t want to cause excess bleeding, so it’s always this delicate balance,” said lead study author Yongzhi Qiu, PhD. “This is the first assay to allow us to really understand what happens during the lifetime of a clot – looking at it from the time it forms, to see how clots get better, either on their own or when adding different clot-busting drugs.”
With this technology, the team engineered microvasculature on a chip. It is similar to when skin cells are cultured on a two-dimensional slide, but here researchers grow endothelial or blood vessel cells in a tissue-like material to form a three-dimensional micro-vessel with branches in a petri dish. The technology models the biophysical microenvironment, such as vessel size, geometry, wall stress, and the tissue stiffness surrounding the blood vessels. The artificial blood vessels are grown over several weeks and the clots are then studied over days to weeks, which mirrors the typical duration seen in patients. The researchers are able to examine how the cellular and biochemical composition of the clot changes and how hemodynamics (blood flow) affect the process.
Dr. Qiu said they have already made some interesting discoveries. For example, inflammation seems to induce protein deposits that initiate clot formation. As clots start to resolve, platelets are mostly undetectable after one day. In addition, if blood vessels are less inflamed, endothelial barrier function restores in one day after the inflammatory insults are removed, and the clots resolve in about 10-14 days. However, if blood vessels are severely inflamed, neutrophils and fibrin persist and may continue to block blood flow and prevent blood vessel cells from recovering. Researchers explained that this may suggest that clinicians do not need to be as hesitant to give anti-platelet therapy before clots form and that not all blood clots are the same.
They said that this assay may warrant broad application in studying thrombosis associated with inflammation that occurs in many conditions such as lupus, rheumatoid arthritis, inflammatory bowel disease, or other autoimmune diseases, as well as many cancers.
“This is the first time we’ve been able to look at the clot for this long of a duration and under these controlled circumstances to model different disease states. What we are learning is that not all clots are created equal, and not all clots should receive the same type of therapy – some therapies are going to be better for certain clots than others,” Dr. Qiu said. “We’re also seeing that certain antithrombotic medications seem to improve the leakiness of the blood vessel cells so not only is it busting the clot, it’s also helping the blood vessel get better.”
He said the implications of this finding are fairly broad because it could mean that even if a person does not have a clot yet, but they have evidence of inflammation, anticlotting medication may play a role in preventing blood clotting and may keep the blood vessel healthier. Clot resolution also appears to be dependent on the extent of inflammation, suggesting that the application of anti-inflammatory medicine might facilitate the clot resolution. Of course, more study is needed.
The researchers say they are hopeful that this assay may help clinicians better target anti-thrombotic and anticoagulant therapies and open new opportunities for therapeutic interventions. They are looking into how to scale the technology for broader use.
This study was funded by grants from the National Institutes of Health.
Yongzhi Qiu, PhD, Emory University School of Medicine will present this study during an oral presentation on Sunday, December 9, at 12 noon in the Sunburst Room.
The study authors and press program moderator will be available for interviews after the press conference or by telephone. Additional press briefings will take place throughout the meeting on sickle cell disease, inclusive medicine, CAR-T and beyond, and late-breaking abstracts. For the complete annual meeting program and abstracts, visit www.hematology.org/annual-meeting. Follow @ASH_hematology and #ASH19 on Twitter and like ASH on Facebook for the most up-to-date information about the 2019 ASH Annual Meeting.
The American Society of Hematology (ASH) (www.hematology.org) is the world’s largest professional society of hematologists dedicated to furthering the understanding, diagnosis, treatment, and prevention of disorders affecting the blood. For 60 years, the Society has led the development of hematology as a discipline by promoting research, patient care, education, training, and advocacy in hematology. ASH publishes Blood (www.bloodjournal.org), the most cited peer-reviewed publication in the field, which is available weekly in print and online. In 2016, ASH launched Blood Advances (www.bloodadvances.org), an online, peer-reviewed open-access journal.
CONTACTS:
Adam Silverstein, FleishmanHillard
917-697-9313; [email protected]
Leah Enser, ASH
202-552-4927; [email protected]