Studies Offer Mix of Hope and Challenges in Addressing Cancer Care Disparities
(Orlando, FL, Dec. 7, 2019) — Five studies being presented today during the 61st American Society of Hematology (ASH) Annual Meeting and Exposition in Orlando paint a mixed portrait of how demographics and socioeconomic status affect access to clinical trials and effective treatments for patients with blood cancers.
Several studies offer encouraging evidence that racial minorities and older patients receive similar benefits from cancer treatments as other patient groups. Other studies, however, show that significant gaps remain in terms of care access and outcomes and underscore the urgent need for renewed efforts to address disparities.
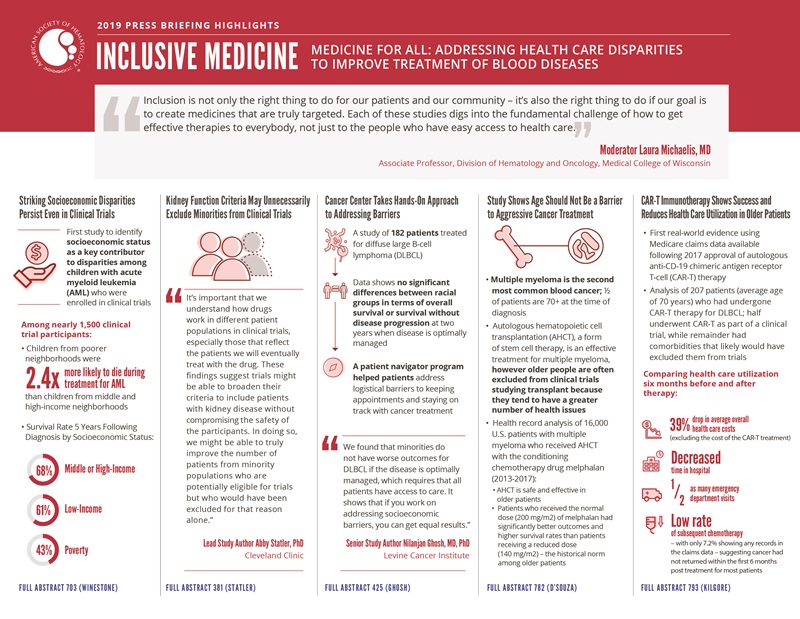
“Inclusion is not only the right thing to do for our patients and our community – it’s also the right thing to do if our goal is to create medicines that are truly targeted,” said press briefing moderator Laura Michaelis, MD, Medical College of Wisconsin. “Each of these studies digs into the fundamental challenge of how to get effective therapies to everybody, not just to the people who have easy access to health care.”
Several studies offer striking insights into the impact of clinical trial inclusion criteria, calling into question criteria that may systematically exclude minorities and older individuals.
“Our ability to achieve tailored treatments and prevention relies on including a wide and heterogenous spectrum of individuals in clinical trials,” said Dr. Michaelis. “We have an obligation to recruit people who are traditionally absent from trials, including groups such as women, older people, minorities, people living in poverty, and people who are chronically ill or who have comorbidities.”
This press conference will take place on Saturday, December 7, at 11:30 a.m. in the ASH press briefing room W221DE.
Striking Socioeconomic Disparities Persist Even in Clinical Trials
#703 Area-Based Socioeconomic Disparities in Survival of Children with Newly Diagnosed Acute Myeloid Leukemia: A Report from the Children’s Oncology Group
Children from poorer neighborhoods were 2.4 times more likely to die during treatment for acute myeloid leukemia (AML) than children from middle and high-income neighborhoods in a study that analyzed nearly 1,500 clinical trial participants. While previous research has pointed to racial disparities in cancer survival, the new study is the first to identify socioeconomic status as a key contributor to disparities among children with AML who were enrolled in clinical trials.
Researchers say the findings are especially alarming given that clinical trials are designed to provide consistent treatment across all participant groups. The fact that disparities were found despite the rigorous setting of clinical trials suggests that these disparities arise from factors outside of the specific chemotherapy used.
“We expected there to be a difference, but the degree of difference is quite substantial,” said lead study author Lena E. Winestone, MD, of the UCSF Benioff Children’s Hospital in San Francisco. “The more people are cognizant about the disparities that exist, the better positioned we’ll be to ameliorate them.”
Researchers at UCSF Benioff Children’s Hospital and the Children’s Hospital of Philadelphia examined clinical trial data from children enrolled on two recent AML trials, AAML1031 and AAML0531, and used U.S. Census data to determine the median income and educational attainment in patients’ neighborhoods. They found that neighborhood socioeconomic factors were significant predictors of survival, even after accounting for insurance type, race, and known biologic risk factors. While about 68% of patients from middle or high-income areas survived for five years following diagnosis, that proportion was 61% among patients from low-income areas and just 43% among patients living in poverty.
A significantly higher proportion of Black and Hispanic patients lived in poverty, low income, and low education areas. Researchers found that the racial disparity persisted even after accounting for neighborhood socioeconomic factors, suggesting Black patients face a significantly higher risk of death than white children living in areas of the same socioeconomic level.
The study did not determine the reasons behind the increased risk of death. One possibility is that toxic stress, which has been linked with lower socioeconomic status, may impact responses to chemotherapy or immune recovery following chemotherapy, Dr. Winestone noted. The researchers plan to further examine when patients died and the cause of death in the hopes of gaining insights as to whether the risks are connected to treatment-related causes or to the cancer itself.
In addition to drawing attention to persistent racial and socioeconomic disparities in cancer outcomes, the results also highlight potential additional data to be collected as part of clinical trials. Rather than relying on neighborhood data as a proxy, Dr. Winestone said it would be helpful if future clinical trials collected individual data on participants’ socioeconomic status at the time of enrollment. “If we could gather that information, it would allow us to dig deeper into the question of how someone’s circumstances outside of the clinical aspects of their disease impact their health outcomes,” said Dr. Winestone.
This study was funded by National Institutes of Health/National Cancer Institute (NIH/NCI) grants to the Children’s Oncology Group, a member of the NCI National Clinical Trials Network.
Lena E. Winestone, MD, UCSF Benioff Children’s Hospital in San Francisco, will present this study during an oral presentation on Monday, December 9 at 10:30 a.m. in Valencia D (W415D).
Kidney Function Criteria May Unnecessarily Exclude Minorities from Clinical Trials
#381 Are Racial Disparities in Acute Myeloid Leukemia (AML) Clinical Trial Enrollment Associated with Comorbidities and/or Organ Dysfunction?
A study of more than 1,000 patients with AML revealed that African Americans were more likely to have evidence of abnormal kidney functioning than whites, but this was not associated with any difference in overall survival. The findings have implications for the design of clinical trials, which typically exclude patients with signs of kidney dysfunction and may disproportionately – and unnecessarily – exclude minorities as a result.
“It’s important that we understand how drugs work in different patient populations in clinical trials, especially those that reflect the patients we will eventually treat with the drug,” said lead study author Abby Statler, PhD, of Cleveland Clinic. “Designers of clinical trials can use data from studies like ours to inform future eligibility criteria in order to test drugs in more diverse populations.”
Clinical trials test the effectiveness of new treatments and identify any safety concerns before a drug can be sold on the market. Trials often seek to enroll patients who have few health problems other than the one being studied (comorbidities), which makes it easier to tell if outcomes are related to the use of the experimental drug rather than influenced by a patient’s other health conditions or medications. However, because patients in racial minorities on average have more comorbidities, this practice may disproportionately exclude these individuals from clinical trials. As a result, the population of trial participants does not reflect the real-world diversity of the patient population who will ultimately receive the drug.
The researchers examined health records from 1,040 AML patients receiving care at Cleveland Clinic from 2003-2019. They found no significant differences between African American and white patients in treatment approaches, rates of responsiveness to treatment, or overall survival, suggesting that treatments worked just as well in African Americans as whites.
However, African Americans were significantly more likely to have abnormal creatinine and creatinine clearance, signs that the kidneys are not clearing waste products from the bloodstream as effectively as they should. These abnormalities, however, may be benign, as previous studies suggest African Americans have higher creatinine levels than whites. Consequently, this laboratory value may falsely underestimate this subpopulation’s kidney function, causing them to fail study enrollment requirements that require normal creatinine or creatinine clearance values.
The study’s finding that patients with minor creatinine or creatinine clearance abnormalities showed no differences in overall survival calls into question the necessity of excluding patients with these abnormalities from AML trials, Dr. Statler said. The study also bolsters evidence that African Americans may simply have higher baseline creatinine levels than white patients.
“These findings suggest trials might be able to broaden their criteria to include patients with kidney disease without compromising the safety of the participants,” said Dr. Statler. “In doing so, we might be able to truly improve the number of patients from minority populations who are potentially eligible for trials but who would have been excluded for that reason alone.”
The study also examined markers for a variety of comorbidities including endocrine, gastrointestinal, liver, cardiovascular, and neurological functioning. Of these, liver dysfunction was the only comorbidity that was associated with diminished survival. The researchers plan to further examine the data to determine precise kidney function cutoff points for future clinical trial eligibility criteria. In addition to AML, Dr. Statler said the study findings could be relevant to designing trials for other cancers, particularly prostate cancer, which disproportionately affects African American men.
Abby Statler, PhD, Cleveland Clinic, will present this study during an oral presentation on Sunday, December 8, at 7:30 a.m. in W307.
Cancer Center Takes Hands-On Approach to Addressing Barriers
#425 Minorities Do Not Have Worse Outcomes for Diffuse Large B-Cell Lymphoma (DLBCL) If Optimally Managed
A study of 182 patients treated for diffuse large B-cell lymphoma (DLBCL) at a safety net cancer center reports that non-Caucasian patients had similar health outcomes to Caucasian patients. The findings contrast with previous population-based studies that have pointed to racial disparities in lymphoma outcomes and suggest possible steps tertiary centers can take to help close the gap.
The Levine Cancer Institute study found no significant differences between racial groups in terms of overall survival or survival without disease progression at two years. Racial groups also had similar rates of relapse, stem cell transplantation, and clinical trial enrollment. While the study does not indicate a specific reason for the lack of disparities, researchers suggest historically underserved patients may have benefitted from hands-on assistance through the institution’s patient navigator program, which was used by 85% of patients in the study.
“The scientific literature shows that racial minorities tend to have poorer outcomes in lymphoma and several other diseases, and we wanted to know if that holds true at our institution,” said senior study author Nilanjan Ghosh, MD, PhD, of Levine Cancer Institute. “We found that minorities do not have worse outcomes for DLBCL if the disease is optimally managed, which requires that all patients have access to care. It shows that if you work on addressing socioeconomic barriers, you can get equal results.”
The center’s patient navigator program is designed to help patients address logistical barriers to keeping appointments and staying on track with their cancer treatment. For example, navigators can help patients who are homeless take advantage of lodging that is available for patients undergoing cancer treatment, or help arrange transportation for patients without a car. Navigators also help coordinate care across providers such as primary care physicians, oncologists, and other specialists.
The researchers analyzed patients treated for newly diagnosed DLBCL between 2016-2019. Roughly four out of five patients identified themselves as Caucasian. Of those identifying as non-Caucasian, about 73% identified as African American, and 15% identified as Hispanic. Caucasians were significantly more likely to have private health insurance and less likely to have government insurance or no insurance than non-Caucasians. Caucasian patients were slightly older than non-Caucasian patients, on average.
Despite the differences in health insurance type, the researchers found Caucasians and non-Caucasians had similar rates of overall survival (74% and 81%, respectively) two years after diagnosis, as well as similar rates of progression-free survival (60% and 63%, respectively). Treatment regimens and outcomes for those with relapsed or refractory DLBCL were also similar among groups.
The researchers will continue to collect data and plan to conduct a larger analysis in the future, including evaluating the relative impact of the patient navigator program.
Bei Hu, MD, Levine Cancer Institute, will present this study during an oral presentation on Sunday, December 8, at 9:30 a.m. in W314.
Study Shows Age Should Not Be a Barrier to Aggressive Cancer Treatment
#782 Breaking the Glass Ceiling of Age in Transplant in Multiple Myeloma
Even though autologous hematopoietic cell transplantation (AHCT), a form of stem cell therapy, is an effective treatment for multiple myeloma, only four out of 10 patients receive this therapy. A new study shows AHCT is safe and effective in older patients and suggests that more people could benefit from the therapy than have typically been offered it.
Older people are often excluded from clinical trials studying transplant because they tend to have a greater number of health issues. Without trials proving newer, aggressive treatments are safe for older patients, doctors may avoid them on the assumption that they are too risky. In addition to showing AHCT is safe and effective in patients over 70 years of age, researchers also found patients fared better when given the conditioning chemotherapy drug melphalan in the normal dose of 200 mg/m2, rather than the reduced dose of 140 mg/m2 often given to older patients.
“This study shows that you can perform these transplants safely in older patients, and the older patients get the same benefits from these treatments as the younger patients do,” said lead study author Anita D’Souza, MD, Medical College of Wisconsin. “In addition, if there are no contraindications other than simply age, it’s worth trying the higher dose of melphalan. Age alone should not be a reason to automatically reduce the dose.”
The study also strengthens the argument that people should not be excluded from clinical trials based on age alone, Dr. D’Souza noted. Multiple myeloma is the second most common blood cancer, and it occurs most often in older adults. Half of patients are age 70 or older at the time of diagnosis.
Using the Center for International Blood and Marrow Transplant Research database, the researchers examined health records of approximately 16,000 patients who received AHCT with melphalan in the United States between 2013-2017. After adjusting for factors such as functional status, comorbidities, and disease stage, they found patients who received their treatments at age 70 or older had similar rates of relapse or disease progression, progression-free survival, and death not caused by a cancer relapse as those 60-69 years of age.
Of patients age 70 and older, about 40% received the full dose of melphalan and 60% received a reduced dose. Those receiving the reduced dose had significantly worse outcomes and lower survival rates. However, Dr. D’Souza noted that it is impossible to determine whether these patients were also more frail to begin with, in which case their poorer outcomes would not necessarily be due to the dosing reduction.
While AHCT specialists often support the use of AHCT in otherwise healthy older patients, Dr. D’Souza said oncologists in community hospitals where many patients are first treated often fail to refer older patients to transplant centers. The researchers noted a significant increase in the proportion of older patients receiving AHCT in 2017 compared to 2013, suggesting that referrals to AHCT specialists increased over time.
In addition to age disparities, the study also speaks to important racial disparities in myeloma care. Myeloma is twice as common in African Americans as whites, yet AHCT rates are significantly lower among black patients. Age likely adds to the barriers for these patients, Dr. D’Souza said.
Pashna Munshi, MD, Georgetown University, will present this study during an oral presentation on Monday, December 9, at 2:45 p.m. in W311ABCD.
CAR-T Immunotherapy Shows Success and Reduces Health Care Utilization in Older Patients
#793 Medicare Patients Receiving Chimeric Antigen Receptor T-Cell Therapy for Non-Hodgkin Lymphoma: A First Real-World Look at Patient Characteristics, Healthcare Utilization and Costs
A new analysis of Medicare claims data provides the first real-world evidence using claims data available after the approval of autologous anti-CD19 chimeric antigen receptor T-cell (CAR-T) therapy, a type of immunotherapy. These analyses show that CAR-T can be beneficial for a broad population of older patients with DLBCL, including those with multiple chronic conditions. The research also shows patients spent less time in the hospital and had lower health care costs after CAR-T than they did in the months leading up to it.
The U.S. Food and Drug Administration (FDA) approved the first CAR T-cell therapy for adults with DLBCL in 2017. However, many of the patients included in the clinical trials leading up to that approval were middle-aged, with a median age of 56-58. This study used the earliest available Medicare claims data to assess the treatment’s use in Medicare patients age 60 and older, who comprise the majority of Medicare beneficiaries and often have multiple chronic health issues.
“Our findings offer evidence that older patients with multiple comorbidities can be treated successfully with CAR-T,” said lead study author Karl M. Kilgore, PhD, of Avalere Health. “While we don’t know the long-term outcomes yet, nearly three-quarters of the patients were still alive six months post-treatment. Even in that narrow window of time we saw a significant decline in health care utilization including hospitalizations and emergency room use, which is suggestive of a successful course of treatment.”
DLBCL, a cancer that starts in the white blood cells, accounts for about one-third of the 74,000 cases of non-Hodgkin lymphoma diagnosed in the United States each year. About 63% of patients survive for five years after their diagnosis. For those who relapse or have refractory disease, treatment options include chemotherapy, stem cell transplantation, and CAR T-cell therapy. CAR-T works by reengineering a patient’s own T cells, part of the immune system, to kill cancer cells. Multiple steps are required to collect, modify, and reinfuse T cells into the patient, a process that is typically combined with lympho-depleting chemotherapy and a single infusion of the patient’s modified T cells.
The researchers analyzed claims data from patients enrolled in Medicare Fee For Service parts A and B October 2017-September 2018. They identified 207 patients with an average age of 70 years who had undergone CAR-T therapy for DLBCL. Half underwent CAR-T as part of a clinical trial, while the remainder had comorbidities that likely would have excluded them from CAR-T clinical trials.
Comparing health care utilization in the six months before and after CAR-T therapy, the researchers found patients’ average overall health care costs dropped by 39% after undergoing CAR-T, excluding the cost of the CAR-T treatment itself. In the months following CAR-T, patients spent less time in the hospital and had half as many emergency department visits than before the therapy. Only 7.2% had any evidence of subsequent chemotherapy in the claims data, suggesting that the cancer had not returned within the first six months following CAR-T for most patients.
The researchers plan to compare the data to patients with private insurance and to a similar group of DLBCL patients who did not receive CAR T-cell therapy to gain further insights into outcomes and costs.
Karl M. Kilgore, PhD, Avalere Health, will present this study during an oral presentation on Monday, December 9, at 2:45 p.m. in Valencia A (W415A).
The study authors and press program moderator will be available for interviews after the press conference or by telephone. Additional press briefings will take place throughout the meeting on VTE, sickle cell disease, CAR-T and beyond, and late-breaking abstracts. For the complete annual meeting program and abstracts, visit www.hematology.org/annual-meeting. Follow @ASH_hematology and #ASH19 on Twitter and like ASH on Facebook for the most up-to-date information about the 2019 ASH Annual Meeting.
The American Society of Hematology (ASH) (www.hematology.org) is the world's largest professional society of hematologists dedicated to furthering the understanding, diagnosis, treatment, and prevention of disorders affecting the blood. For 60 years, the Society has led the development of hematology as a discipline by promoting research, patient care, education, training, and advocacy in hematology. ASH publishes Blood (www.bloodjournal.org), the most cited peer-reviewed publication in the field, which is available weekly in print and online. In 2016, ASH launched Blood Advances (www.bloodadvances.org), an online, peer-reviewed open-access journal.
Contacts:
Adam Silverstein, FleishmanHillard
917-697-9313; [email protected]
Leah Enser, ASH
202-552-4927; [email protected]