New Approaches Aim to Enhance CAR TCell Therapy
(Orlando, FL, Dec. 7, 2019) –– Four early-phase studies being presented today during the 61st American Society of Hematology (ASH) Annual Meeting and Exposition spotlight the rapid advances being made in cellular immunotherapy for blood cancers. Researchers will present the results of early-phase studies of emerging “second-generation” cellular immunotherapy products that strive to overcome the limitations of existing products.
Cellular immunotherapy uses genetic engineering to enhance the ability of the immune system – the body’s defense system against infection and disease – to kill malignant cells in the blood, the bone marrow, and other sites, in order to keep cancer from coming back. Chimeric antigen receptor T-cell (CAR-T) therapies are developed by harvesting a patient’s own T cells (the immune system’s primary cancer-killing cells), engineering them to target proteins specific to the surface of cancer cells, and reintroducing these modified T cells back into the patient’s immune system to kill the cancer cells.
First-generation CAR T-cell therapies primarily target CD-19, a protein found on the surface of most normal and malignant B cells in B cell cancers such as lymphoma. These therapies have been shown to produce long-term remissions in about one-third of patients with B-cell lymphomas that have not responded to prior therapies.
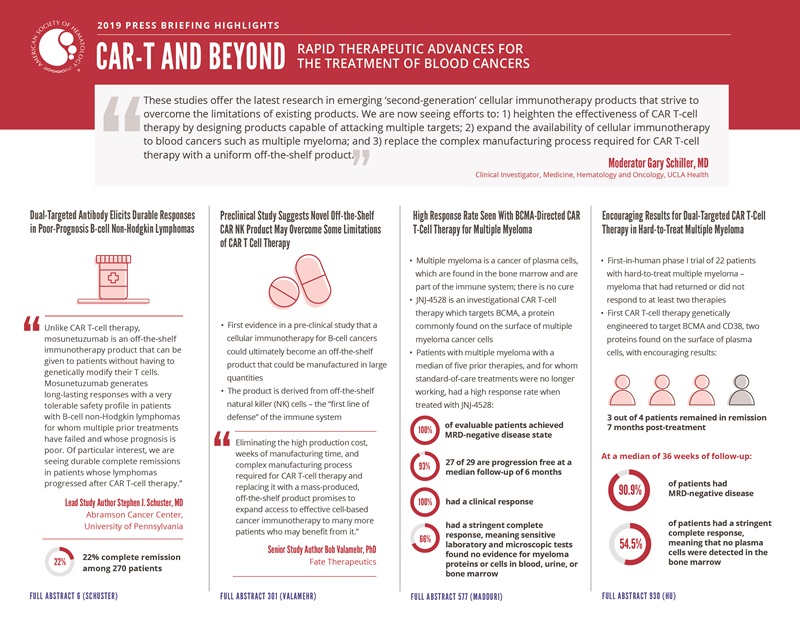
“We are now seeing efforts to: 1) enhance the effectiveness of CAR T-cell therapy by designing products capable of attacking multiple targets; 2) expand the availability of cellular immunotherapy to other blood cancers such as multiple myeloma; and 3) replace the complex manufacturing process required for CAR T-cell therapy with a uniform off-the-shelf product,” said press briefing moderator Gary Schiller, MD, UCLA Health.
One phase I study to be presented today evaluates an off-the-shelf cellular immunotherapy product that targets two proteins found on the surface of lymphoma cells, including its potential to “revive” previously administered CAR T cells that have stopped working. Another study presents preclinical results for one of the first cellular immunotherapies to be based on off-the-shelf natural killer (NK) cells and the first, according to its manufacturer, to be genetically engineered to contain three active anti-tumor components.
The other two studies, also phase I studies, assess novel CAR T-cell therapies for multiple myeloma that test different dual-target strategies. One product is genetically engineered to contain two proteins that attach to BCMA, a protein found almost exclusively on the surface of plasma cells, the immune-system cells that become cancerous in multiple myeloma. The other is designed to target both BCMA and CD-38, another protein found on the surface of plasma cells. In both studies, many patients achieved minimal residual disease (MRD) negativity, which means that using highly sensitive testing fewer than one myeloma cell per 100,000 cells was identified in the bone marrow. Previous studies have shown that patients who achieve this milestone have a lower risk of relapse after more than three years of follow-up.
The three phase I studies also hint at the possibility that dual-targeted CAR T-cell therapies might result in fewer patients experiencing moderate to severe cytokine release syndrome (CRS), a known adverse effect caused by an immune response in the body to the activated T cells that are attacking the cancer. CRS causes flu-like symptoms such as fever, body aches, and fatigue, and in severe cases can be life-threatening. Treatment with the drug tocilizumab can reduce CRS symptoms.
This press conference will take place on Saturday, December 7, at 7:30 a.m. in the ASH press briefing room W221DE.
Dual-Targeted Antibody Elicits Durable Responses in Poor-Prognosis non-Hodgkin Lymphoma (NHL)
#6 Mosunetuzumab Induces Complete Remissions in Poor Prognosis Non-Hodgkin Lymphoma Patients, Including Those Who Are Resistant to or Relapsing after Chimeric Antigen Receptor T-Cell (CAR-T) Therapies, and Is Active in Treatment through Multiple Lines
Patients with B-cell NHL that had returned after or failed to respond to a median of three prior therapies showed complete responses and durable remissions after being treated with an investigational drug called mosunetuzumab. Among patients whose lymphoma progressed after treatment with CAR T-cell therapy, 22% had complete remissions when treated with mosunetuzumab. This new drug targets two proteins, one on the surface of tumor cells and the other on the surface of the recipient’s Tcells.
“Unlike CAR T-cell therapy, mosunetuzumab is an off-the-shelf immunotherapy product that can be given to patients without having to genetically modify their T cells,” said lead author Stephen J. Schuster, MD, of Abramson Cancer Center at the University of Pennsylvania in Philadelphia. “Mosunetuzumab generates long-lasting responses with a very tolerable safety profile in patients with B-cell non-Hodgkin lymphomas for whom multiple prior treatments have failed and whose prognosis is poor. Of particular interest, we are seeing durable complete remissions in patients whose lymphomas progressed after CAR-T.”
Many remissions continue after patients stop receiving the drug. “I have stopped therapy in some patients after six months and they have remained in remission. Some patients have remained in remission without additional therapy for more than a year,” Dr. Schuster said.
New treatment options are needed not only for patients in whom CAR T-cell therapy has failed, but also for those patients whose lymphomas are getting worse so quickly that they cannot wait for CAR T cell manufacturing, which takes several weeks, Dr. Schuster said.
Mosunetuzumab is a synthetic antibody designed to bind to a specific marker on tumor cells. It works by activating the patient’s own T cells, stimulating them to attack and kill cancerous B cells to which they have been introduced by the novel antibody. The drug could potentially be given to patients before, after, or in combination with CAR-T, which needs to be further tested and explored, researchers explained.
Data were presented for 270 patients (median age 62, 172 men) enrolled in the phase I trial in seven countries (the United States, Australia, Canada, Germany, South Korea, Spain, and the United Kingdom). All had B-cell lymphomas that had come back or not responded to a median of three prior therapies. Two-thirds of patients (67%) had fast-growing lymphomas; 85 (31%) patients had more slow-growing forms of the disease. In 30 patients (11%), the cancer was resistant to or returned after an initial response to CAR T-cell therapy; in 77 patients (29%), the disease had progressed after a stem cell transplant.
All patients were treated with mosunetuzumab by intravenous infusion. They had an imaging test at either six weeks or three months after starting therapy to assess the initial response to treatment, and responses continued to be followed every three months thereafter.
Forty-six of 124 patients with fast-growing lymphomas (37%) had measurable decreases in the extent of their cancer (objective response); 24 of 124 patients (19%) saw all detectable tumors disappear (complete response). A higher response rate was observed in patients with higher exposure to mosunetuzumab. Among patients with slow-growing lymphomas, 42 of 67 (63%) had objective responses and 29 of 67 (43%) had complete responses. Both objective response rate and complete response rate were maintained in subgroups of patients at high risk for relapse.
Complete remissions appear to be long lasting, Dr. Schuster said. With a median follow-up of six months since first complete remission, 24 of 29 patients (83%) who achieved complete remissions of their slow-growing lymphomas and 17 of 24 patients (71%) who achieved complete remissions of their fast-growing lymphomas remain free of disease. In some patients whose cancers progressed after receiving CAR T-cell therapy, highly sensitive molecular testing showed that the previously administered CAR T cells increased in number. This suggests that, in addition to its ability to kill cancerous B cells, mosunetuzumab may also help augment the effect of the prior CAR-T treatment, Dr. Schuster said.
In this study, 29% of patients treated with mosunetuzumab experienced cytokine-release syndrome that was mostly mild. In 3% of patients, CRS was treated with tocilizumab. Four percent of patients experienced moderately severe neurologic side effects. Patients who received higher doses of mosunetuzumab were no more likely to have CRS or neurologic side effects than patients treated at lower doses.
A study of a higher dose of mosunetuzumab is now enrolling patients, Dr. Schuster said. Long-term follow-up of these patients will ultimately help to better evaluate the durability of response data.
“Larger, randomized trials are needed to further confirm these promising data and determine whether the treatment benefit of mosunetuzumab is enhanced when it is used earlier in the course of lymphoma therapy or in combination with other agents,” Dr. Schuster said.
This study was supported by Genentech, Inc.
Stephen J. Schuster, MD, Abramson Cancer Center, University of Pennsylvania will present this study during the plenary session on Sunday, December 8, at 2 p.m. in Hall D.
Novel Off-the-Shelf CAR NK Product Overcomes CD19 Antigen Escape in Preclinical Studies
#301 FT596: Translation of First-of-Kind Multi-Antigen Targeted Off-the-Shelf CAR NK Cell with Engineered Persistence for the Treatment of B Cell Malignancies
Preclinical studies provide the first evidence that cellular immunotherapy for B cell cancers could ultimately become an off-the-shelf product, capable of being uniformly manufactured in large quantities as prescription drugs are.
“We have taken the concept of traditional pharmaceutical drug development and applied it to cellular therapy,” said senior author Bob Valamehr, PhD, of Fate Therapeutics, a San Diego biopharmaceutical company.
The product, dubbed FT596, is among the first cellular immunotherapies to be based on off-the-shelf NK cells – the “first line of defense” of the immune system – and is the first cellular immunotherapy to be genetically engineered to contain three active anti-tumor components, according to Dr. Valamehr.
FT596 demonstrated comparable ability to kill cancerous white blood cells as standard CAR T cells and, when combined with the drug rituximab, killed cancerous white blood cells that were no longer responding to standard CAR T-cell therapy due to loss of the CD19 antigen target.
The U.S. Food and Drug Administration (FDA) approved Fate Therapeutics’ Investigational New Drug Application for FT596 in September and the company hopes to begin a first-in-human phase I clinical trial for the treatment of B-cell lymphoma and chronic lymphocytic leukemia in the first quarter of 2020. The primary purpose of this trial will be to assess the safety and activity of FT596 in patients.
The process of creating FT596 begins with human induced pluripotent stem cells (iPSCs) that are uniquely capable of unlimited self-renewal and can differentiate into more than 200 types of human cells. The iPSCs are genetically engineered, after which a single clone (genetically engineered cell) is selected and multiplied in the laboratory to create a master engineered cell line that can be repeatedly used to generate cancer-fighting immune-system cells such as NK and T cells.
NK cells are part of the innate immune system, the body’s first line of defense against infection and disease. Unlike T cells, which have to be trained to recognize their target and can kill only cells that display that target on their surface, NK cells do not need special preparation before going on the attack and can kill many different types of transformed or infected cells.
“NK cells are multifaceted and can be viewed as a ‘jack-of-all-trades’ when it comes to protecting the host, whereas T cells can act in only one way,” explained Dr. Valamehr.
But NK cells are unlike T cells in a couple of other ways: They are inherently limited in their capacity to multiply and expand when infused into patients, and they have a shorter lifespan.
Dr. Valamehr and his colleagues used genetic engineering to address these shortcomings. In addition to engineering FT596 to carry a CAR targeting the CD19 protein – which is produced by nearly all B-cell lymphomas and leukemias – they inserted two other novel proteins: CD16, which boosts and broadens the NK cells’ ability to kill cancer cells, and IL15, which stimulates FT596 to proliferate and persist.
FT596 has been designed to address two other limitations of CAR T-cell therapy, said Dr. Valamehr.
- As an off-the-shelf product, it significantly improves the current patient-by-patient CAR-T treatment paradigm by eliminating the time-consuming and costly process that is currently required to treat a patient with CAR T cells (harvesting the patient’s own T cells, sending those cells to a manufacturing site to be genetically engineered, processing the manufactured product for shipment back to the treating hospital, and finally infusing the CAR T cells into the patient).
- The addition of the CD16 protein gives FT596 broader therapeutic activity and versatility. In combination with a drug such as rituximab, FT596 has the potential to lead to deeper and more durable responses and overcome resistance that hampers the long-term efficacy of CAR T-cell therapy.
“Eliminating the high production cost, weeks of manufacturing time, and complex manufacturing process required for CAR T-cell therapy and replacing it with a mass-produced, off-the-shelf product promises to expand access to effective cell-based cancer immunotherapy to many more patients who may benefit from it,” said Dr. Valamehr.
This study was supported by Fate Therapeutics, Inc.
Jode P. Goodridge, PhD, Fate Therapeutics, will present this study during an oral presentation on Saturday, December 7 at 4 p.m. in Valencia A (W415A).
High Response Rate Seen With BCMA-Directed CAR T-Cell Therapy for Multiple Myeloma
#577 Results from CARTITUDE-1: A Phase 1b/2 Study of JNJ-4528, a CAR T-Cell Therapy Directed Against B-Cell Maturation Antigen (BCMA), in Patients with Relapsed and/or Refractory Multiple Myeloma (R/R MM)
Patients with multiple myeloma who had received a median of five prior therapies, and for whom standard-of-care treatments were no longer working, had a high response rate when treated with the investigational CAR T-cell therapy JNJ-4528, which targets BCMA, a protein commonly found on the surface of multiple myeloma cancer cells.
“We are seeing a high response rate, with most patients achieving MRD negativity,” said lead study author Deepu Madduri, MD, of The Tisch Cancer Institute at Mount Sinai in New York. “Considering these patients have all received multiple prior therapies, these results are extremely encouraging.”
All evaluable patients receiving this CAR T-cell therapy have achieved MRD-negative disease state and 27 of 29 patients are progression free at a median follow-up of six months, Dr. Madduri said.
Multiple myeloma is a cancer of plasma cells, which are found in the bone marrow and are part of the immune system, the body’s defense system against infection. Typical signs and symptoms of multiple myeloma may be bone pain or fractures, high levels of calcium in the blood, kidney damage, and anemia. Multiple myeloma affects an estimated 160,000 people each year, occurs most often in people over 60, and is slightly more common in men than in women.
Although new therapies for multiple myeloma have recently become available that can extend patients’ life expectancy, a cure for the disease remains elusive, Dr. Madduri said. “We can get the disease into remission, but most patients unfortunately relapse, and outcomes are very poor for patients who have relapsed multiple times,” she said.
Researchers said that JNJ-4528 is a novel CAR T-cell therapy featuring two molecules that bind to BCMA, a protein found on the surface of multiple myeloma cells. “We are learning that every CAR T-cell therapy is different,” said Dr. Madduri. “JNJ-4528 has a unique CAR T cell composition in patients, preferentially enriched in CD8 T cells, which are believed to be one of the most important T cells in killing cancer cells.”
This phase Ib/II trial is continuing to enroll patients. Dr. Madduri reported results for the first 29 patients enrolled. Patients’ T cells were collected and sent to a laboratory where they were genetically engineered to express JNJ-4528. Prior to reinfusing these CAR T cells, the patients received three days of chemotherapy to “make room” in their immune systems for the engineered T cells. Following chemotherapy, each patient received a single infusion of the JNJ-4528 CAR T cells. They had blood and bone marrow exams at a minimum at 28 days, six months, and one year after treatment to assess their response. The primary aims of the trial are to assess the therapy’s safety and to confirm the dose to be tested in a larger, phase II trial.
The median follow-up time in the current analysis is six months. Overall, 100% of patients had a clinical response to JNJ-4528. Moreover, 66% had a stringent complete response, meaning that sensitive laboratory and microscopic tests found no evidence for myeloma proteins or cells in blood, urine, or bone marrow.
Most patients (93%) experienced CRS; one patient had severe (grade 3) CRS, and one patient died from its complications 99 days after the CAR T cell infusion. In 76% of patients, CRS was treated with tocilizumab.
“To see some patients in this heavily pretreated population surviving for a year or more with a one-time treatment and a manageable safety profile is remarkable,” Dr. Madduri said. “These patients feel that they have their quality of life back. They no longer have to come into the clinic for weekly treatments and some are well enough to travel.”
The phase II portion of this study is ongoing to evaluate the overall response rate of patients treated with JNJ-4528. Additional clinical studies are evaluating the safety and efficacy of JNJ-4528 in different multiple myeloma treatment settings.
This study was supported by Janssen Research & Development, LLC.
Deepu Madduri, MD, Tisch Cancer Institute, Mount Sinai will present this study during an oral session on Monday, December 9, at 6:15 p.m. in Valencia A (W415A).
Encouraging Results for Dual-Targeted CAR T-Cell Therapy in Hard-to-Treat Multiple Myeloma
#930 A Bispecific CART-Cell Therapy Targeting BCMA and CD38 for Relapsed/Refractory Multiple Myeloma: Updated Results from a Phase I Dose-Climbing Trial
More than three out of four patients with multiple myeloma that returned or did not respond to at least two therapies remained in remission seven months after treatment with a novel CAR T-cell therapy targeting two proteins that are frequently found on myeloma cells. Those experiencing sustained remissions include nine patients with a difficult-to-treat form of multiple myeloma in which the disease has spread beyond the bone marrow.
Roughly one in 10 patients with multiple myeloma develop tumors in the organs or soft tissues such as the blood vessels, muscles, and nerves. These so-called extramedullary tumors respond poorly to treatment, and patients who develop them have a poor outlook and poor quality of life, said study author Yu Hu, MD, PhD, of Union Hospital, Huazhong University of Science and Technology in Wuhan, China.
“Our results show that this CAR T-cell product can effectively achieve elimination of extramedullary tumors,” said Dr. Hu. “Although these are preliminary data, they are encouraging for patients with multiple myeloma who have not responded to other therapies.”
The study treatment is the first CAR T-cell therapy to be genetically engineered to target BCMA and CD38, two proteins found on the surface of plasma cells. Multiple myeloma is a cancer of plasma cells, which are found in the bone marrow and are part of the immune system, the body’s defense system against infection and disease.
“Our thinking was that targeting both of these proteins would improve treatment efficacy without increasing toxicity, and induce deeper, more durable remissions,” said Dr. Hu.
The first-in-humans phase I trial enrolled 22 patients whose average age was 59, of whom 11 were men. All had multiple myeloma that had returned or not responded to at least three therapies. Nine of the 22 patients had extramedullary tumors. The study aims were to determine the safest and most effective dose of the CAR T-cell therapy as well as to initially evaluate its effectiveness.
Patients received three days of chemotherapy to “make room” in their immune systems for the engineered T cells. Then each patient was infused with the dual-targeted CAR T cells. Patients were divided into five groups, with each group receiving a higher dose than the previous one. Depending on the cell dose, patients received either one or two infusions.
At a median of 36 weeks of follow-up, 18 patients (90.9%) had MRD-negative disease. Twelve patients (54.5%) had a stringent complete response, meaning that no plasma cells were detected in the bone marrow. Seven patients (31.8%) had a good or very good partial response, meaning that the level of M-protein (an abnormal protein produced by cancerous plasma cells) in the blood or urine was reduced but still detectable. In eight of the nine patients with extramedullary lesions, these tumors were undetectable on their computed tomography scans. For the 17 patients who remained in remission at seven months after treatment, the median duration of response was 28.8 weeks.
Researchers observed some side effects: 20 patients experienced CRS, of whom six needed treatment. No serious adverse neurologic effects such as seizures, movement impairment, difficulty speaking or understanding speech, or fatal swelling in the brain were reported.
“With this dual-targeted CAR T-cell therapy, we have demonstrated a high response rate, especially a higher rate and longer duration of stringent complete response, compared with other therapies, as well as effective elimination of extramedullary lesions, with no serious neurologic adverse effects and manageable levels of other adverse effects,” said Dr. Hu.
The investigators will continue to follow the patients for two years. They are also planning to conduct a phase II trial in both China and the United States to test the treatment’s effectiveness in a larger number of patients.
This study was supported by the National Natural Science Foundation of China, the Major Technological Innovation Special Project fund of Hubei Province of China, and Cellyan Therapeutics Co., Ltd.
Yu Hu, MD, PhD, Union Hospital, Huazhong University of Science and Technology, will present this study during an oral presentation on Monday, December 9, at 6:15 p.m. in Hall D.
The study authors and press program moderator will be available for interviews after the press conference or by telephone. Additional press briefings will take place throughout the meeting on VTE, sickle cell disease, inclusive medicine, and late-breaking abstracts. For the complete annual meeting program and abstracts, visit www.hematology.org/annual-meeting. Follow @ASH_hematology and #ASH19 on Twitter and like ASH on Facebook for the most up-to-date information about the 2019 ASH Annual Meeting.
The American Society of Hematology (ASH) (www.hematology.org) is the world’s largest professional society of hematologists dedicated to furthering the understanding, diagnosis, treatment, and prevention of disorders affecting the blood. For 60 years, the Society has led the development of hematology as a discipline by promoting research, patient care, education, training, and advocacy in hematology. ASH publishes Blood (www.bloodjournal.org), the most cited peer-reviewed publication in the field, which is available weekly in print and online. In 2016, ASH launched Blood Advances (www.bloodadvances.org), an online, peer-reviewed open-access journal.
Contacts:
Adam Silverstein, FleishmanHillard
917-697-9313; [email protected]
Leah Enser, ASH
202-552-4927; [email protected]