New Therapies Improve Outlook for Bleeding and Clotting Disorders
Novel drugs and gene therapy show promising results in trials for patients with hemophilia A and cancer
(Atlanta, December 9, 2017) — In three studies being presented today during the 59th American Society of Hematology (ASH) Annual Meeting and Exposition in Atlanta, researchers report remarkable benefits from new, more easily administered therapies for bleeding and clotting disorders.
Two studies, one involving a novel drug and the other a gene therapy, could significantly improve the lives of people with the bleeding disorder hemophilia A, the most common form of the disease. For children with hemophilia A who develop resistance to the standard, but burdensome, intravenous therapy, subcutaneous administration of the investigational drug emicizumab effectively prevents bleeds. For adults with hemophilia A, a single gene therapy treatment provides durable improvement in clotting factor levels and long-term protection from bleeds.
A third study shows that the direct oral anti-coagulant (DOAC) rivaroxaban appears to safely reduce the risk of recurrent, dangerous blood clots in patients with cancer, even during chemotherapy.
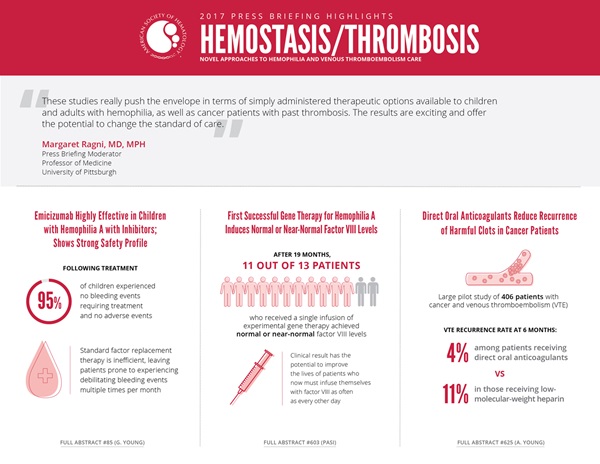
“These studies really push the envelope in terms of simply-administered therapeutic options available to children and adults with hemophilia, as well as cancer patients with a history of blood clots,” said Margaret Ragni, MD, MPH, press briefing moderator, professor of medicine at the University of Pittsburgh. “The results are exciting and offer the potential to change the standard of care.”
This press conference will take place on Saturday, December 9, at 7:30 a.m. EST in Room A315 of the Georgia World Congress Center.
Emicizumab Highly Effective in Children with Hemophilia A with Inhibitors; Shows Strong Safety Profile
HAVEN 2 Updated Analysis: Multicenter, Open-Label, Phase 3 Study to Evaluate Efficacy, Safety, and Pharmacokinetics of Subcutaneous Administration of Emicizumab Prophylaxis in Pediatric Patients with Hemophilia A with Inhibitors [85]
In a Phase III trial of the hemophilia A drug emicizumab in children, 95 percent of patients experienced no bleeding events requiring treatment, suggesting the drug is highly effective at preventing the bleeding associated with hemophilia A. The findings also reveal a strong safety profile, with no serious adverse events related to the drug, according to the research team.
People with hemophilia A produce extremely low levels of the blood clotting protein factor VIII (FVIII). Without treatment, patients can suffer debilitating bleeding events multiple times per month, especially in the joints, causing significant pain in the short term and joint disease in the long term. The best available treatment for preventing bleeds involves frequent intravenous infusions of FVIII.
In some patients, these infusions do not work because the body develops antibodies, or inhibitors, that bind to the standard replacement therapy and render it ineffective. Emicizumab is designed to fill the treatment gap for these patients. The drug functions like FVIII by enabling blood to clot, but it has a different structure, making it unrecognizable to FVIII antibodies.
Researchers enrolled 60 patients age one to 12 years who had an inhibitor that prevented them from being effectively treated with FVIII infusions. Caregivers were taught how to administer emicizumab at home through a weekly subcutaneous (under the skin) injection. Over a median of nine weeks follow-up (with a range of 1 to 41 weeks), only three patients experienced bleeding events requiring treatment; all three were safely treated with recombinant factor VIIa (rFVIIa), a standard of care for people with hemophilia A and an inhibitor. Known as a bypassing agent, rFVIIa encourages coagulation without the need for FVIII replacement therapy, providing a therapeutic workaround for those who have developed FVIII inhibitors.
“Before this drug, we didn’t have very effective ways to prevent joint bleeding in these patients,” said lead study author Guy Young, MD, director of the hemostasis and thrombosis program at Children’s Hospital Los Angeles and University of Southern California. “This drug has demonstrated a very high level of efficacy at preventing those bleeding events. It’s been life-changing for the children I’ve treated.”
Previous emicizumab trials conducted in adults and adolescents have raised safety concerns over adverse events that occurred after patients experienced bleeding while on the drug, which Dr. Young attributed to the concomitant use of a bypassing agent on top of emicizumab. He said such problems had not occurred in this trial, likely in large part due to the fact that the patients on this trial rarely used bypassing agents since they had so few bleeding events.
The researchers will continue to follow enrolled patients for at least 12 months. Dr. Young says the trial’s findings could change the standard of care for children who have hemophilia A with inhibitors. Another trial is underway to determine the safety and efficacy of emicizumab in patients who do not have the inhibitors.
Emicizumab is co-developed by Roche and Genentech.
Guy Young, MD, of Children’s Hospital Los Angeles, will present this study during an oral presentation on Saturday, December 9, at 9:30 a.m. EST in Room B207 of the Georgia World Congress Center.
First Successful Gene Therapy for Hemophilia A Induces Normal or Near-Normal Factor VIII Levels
Achievement of Normal Circulating Factor VIII Activity Following BMN 270 AAV5-FVIII Gene Transfer: Interim, Long-Term Efficacy and Safety Results from a Phase 1/2 Study in Patients with Severe Hemophilia A [603]
Patients with hemophilia A who received a single infusion of an investigational gene therapy showed improved levels of the essential blood clotting protein FVIII, with 11 of 13 achieving normal or near-normal FVIII levels, according to the latest data from a trial that followed patients for up to 19 months. Researchers state that this represents the first successful gene therapy trial for people with hemophilia A.
The therapy uses a viral vector to transfer a functional copy of the gene responsible for producing FVIII, which is mutated in people with hemophilia A, into the patient’s body.
Data were reported on two dosing levels. After several weeks, all patients began producing FVIII. By 20 weeks after the infusion, median FVIII levels in those receiving the higher dose plateaued and remained within the normal range. Those receiving the lower dose had FVIII levels that increased steadily to a median of 34 IU/dL by 20 weeks and, in the three patients who had been followed for 32 weeks, a median of 51 IU/dL — a level that is within the normal range and represents a dramatic increase over their pre-treatment FVIII levels of less than 1 IU/dL.
In contrast to standard care, which requires multiple intravenous therapy infusions per week, this gene therapy appears to have long-lasting effects after a single infusion.
Prior to this study, participants received up to 185 FVIII infusions per year to prevent bleeds, resulting in up to 41 breakthrough bleeding episodes per year despite prophylactic treatment. After receiving the gene therapy, all patients from both dose cohorts were able to completely discontinue prophylactic FVIII infusions, and 10 had no bleeding episodes requiring FVIII treatment from four weeks after infusion through the last follow-up visit. No patients showed evidence of an adverse response by the immune system, a side effect that has posed concern in trials for other gene therapies.
While several gene therapies have shown success for the rarer form, hemophilia B, gene therapy for hemophilia A has been considered more challenging because it is associated with a complex and much larger gene, making successful gene therapy considerably more difficult.
“The clinical data to date for this investigational gene therapy exceeded our expectations, in terms of increasing factor VIII levels and reducing the annualized bleed rate,” said lead researcher K. John Pasi, MD, professor of hemostasis and thrombosis at Barts and the London School of Medicine and Dentistry and haemophilia clinical director at Barts Health NHS Trust. “Many clinical trial participants have seen factor VIII levels at or close to normal. This clinical result has the potential to improve the lives of patients who now must infuse themselves with factor VIII as often as every other day. With this experimental treatment, we are researching whether it may be possible for hemophilia A patients to reduce or eliminate factor VIII treatment over an extended timeline.”
This study was supported by BioMarin Pharmaceutical, Inc.
K. John Pasi, MD, Barts and the London School of Medicine and Dentistry, will present this study during an oral presentation on Monday, December 11, at 7:00 a.m. EST in Auditorium C101 of the Georgia World Congress Center.
Direct Oral Anticoagulant Reduces Recurrence of Harmful Clots in Patients with Cancer
Anticoagulation Therapy in Selected Cancer Patients at Risk of Recurrence of Venous Thromboembolism: Results of the ‘Select-D’ Pilot Trial [625]
People with cancer have an increased risk of developing blood clots, with roughly one in five experiencing venous thromboembolism (VTE) — blood clots that occur in deep veins like the legs or that travel through the blood stream and get lodged in the small blood vessels in the lungs. International guidelines recommend treatment using low-molecular-weight heparin, an anticoagulant that is injected subcutaneously; however, new results from a large pilot trial suggest that DOACs, newer blood thinners administered as a daily pill, could be a safe and beneficial alternative for treating VTE in selected patients.
Although there are many causes and risk factors for VTE, its increased prevalence in cancer patients is thought to be related to a combination of factors such as immobility from remaining in bed, procoagulants produced by the tumor, and chemotherapy. Because VTE can be life-threatening, blood thinners are used to shrink existing clots and prevent others from forming.
The select-d trial enrolled 406 patients who had cancer and VTE; most (69 percent) were receiving cancer treatment (typically chemotherapy) at the time of their VTE. Half were randomly assigned to receive low-molecular-weight heparin (dalteparin) and half were assigned to receive a DOAC (rivaroxaban). After six months of treatment, the VTE recurrence rate was four percent among those receiving the DOAC and 11 percent in those receiving dalteparin.
The results for secondary outcomes were mixed. In patients receiving the DOAC, there were more major bleeding events (11 patients) and a marked increase in clinically relevant non-major bleeds (25 patients) compared to those taking heparin (6 and 6 patients, respectively). The researchers are conducting further analyses to try to understand factors that may have contributed to this difference.
“Clinicians are already adopting DOACs into practice for these patients,” said lead study author Annie Young, PhD, Professor of Nursing at the University of Warwick, “and now they have data from this study to indicate that DOACs are potentially safe in cancer patients. We need to be looking at different groups of people and different types of bleeds in more detail, so that we can choose the best treatment for each patient.”
This study was supported by an unrestricted grant from Bayer AG.
Annie Young, PhD, University of Warwick, United Kingdom, will present this study during an oral presentation on Monday, December 11, at 10:30 a.m. EST in Room B207 of the Georgia World Congress Center.
The study authors and press program moderator will be available for interviews after the press conference or by telephone. Additional press briefings will take place throughout the meeting. For the complete annual meeting program and abstracts, visit http://www.hematology.org/annual-meeting. Follow @ASH_hematology and #ASH17 on Twitter and like ASH on Facebook for the most up-to-date information about the 2017 ASH Annual Meeting.
The American Society of Hematology (www.hematology.org) is the world’s largest professional society of hematologists dedicated to furthering the understanding, diagnosis, treatment, and prevention of disorders affecting the blood. For more than 50 years, the Society has led the development of hematology as a discipline by promoting research, patient care, education, training, and advocacy in hematology. ASH publishes Blood (www.bloodjournal.org), the most cited peer-reviewed publication in the field, which is available weekly in print and online. In 2016, ASH launched Blood Advances (www.bloodadvances.org), an online, peer-reviewed open-access journal.
CONTACTS:
Stephen Fitzmaurice, ASH
561-506-6890; [email protected]
Adam Silverstein, FleishmanHillard
917-697-9313; [email protected]