Late-Breaking Clinical Trials Signal New Therapeutic Options for Many Patients in the Near Term
(Atlanta, December 12, 2017) — In four clinical trials being presented today during the 59th American Society of Hematology (ASH) Annual Meeting and Exposition in Atlanta, researchers report promising results suggesting patients with blood disorders and several types of cancer will soon have significantly expanded options for treatment. The announcements reflect the latest results from clinical trial data collected and analyzed within the past few months.
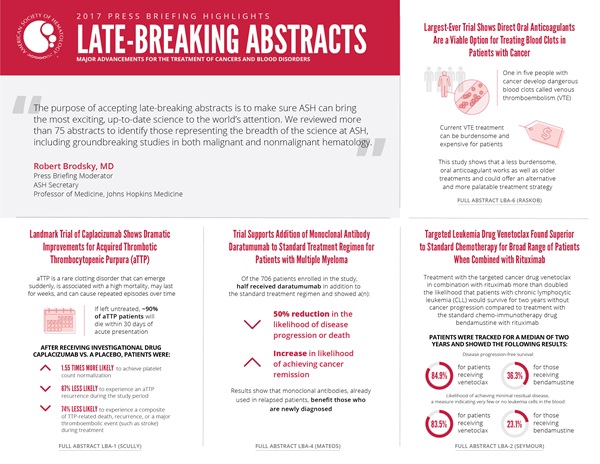
“The purpose of accepting late-breaking abstracts is to make sure that ASH can bring the most exciting, up-to-date science to the world’s attention,” said press briefing moderator Robert Brodsky, MD, ASH Secretary and professor of medicine at Johns Hopkins Medicine. “We reviewed more than 75 abstracts to identify those that are presenting the breadth of the science at ASH, including groundbreaking studies in both malignant and nonmalignant hematology.”
The first study addresses the use of direct oral anticoagulants (DOACs) to safely treat dangerous blood clots in patients with cancer. The second reports a significant breakthrough for reducing risks during the most acute period of the rare blood disorder thrombotic thrombocytopenic purpura (TTP). In the third and fourth studies, new drugs show remarkable improvements over standard care for multiple myeloma and chronic lymphocytic leukemia, respectively.
This press conference will take place on Monday, December 11, at 10:30 a.m. EST in Room A315 of the Georgia World Congress Center.
Largest-Ever Trial Shows Direct Oral Anticoagulants Are a Viable Option for Treating Blood Clots in Patients with Cancer
A Randomized, Open-Label, Blinded Outcome Assessment Trial Evaluating the Efficacy and Safety of LMWH/Edoxaban Versus Dalteparin for Venous Thromboembolism Associated with Cancer: Hokusai VTE-Cancer Study [LBA-6]
People with cancer face an increased risk for venous thromboembolism (VTE), blood clots that occur in deep veins like the legs or that travel through the blood stream and get lodged in the small blood vessels in the lungs. Under current guidelines, cancer patients who develop VTE are prescribed low-molecular-weight heparin, an anticoagulant that must be injected under the skin daily for several months. While effective, this regimen can be expensive and often burdensome for patients, leading many to prematurely discontinue treatment.
Results from the first large randomized controlled trial comparing this standard blood-thinning treatment with newer anticoagulants, DOACs, suggest the DOAC known as edoxaban — taken as a daily pill — work as well as low-molecular-weight heparin and could, therefore, offer an alternative and potentially more palatable treatment strategy, according to researchers.
Roughly one out of five people with cancer develop VTE, which can cause pain and swelling when clots occur in deep veins (known as deep vein thrombosis) and breathing problems, chest pain and even death if they move into the lungs (known as pulmonary embolism). Anticoagulants prevent the growth of existing clots and prevent others from forming, but these drugs also elevate the risk of bleeding. Doctors must therefore balance the risks of recurrent clots against the risks of bleeding when treating VTE.
This study enrolled 1,050 individuals with cancer being treated for VTE at 114 centers in 13 countries. Patients represented a wide range of cancer types and chemotherapy regimens; about 10 percent had blood cancers and the rest had solid tumors. Half were randomly assigned to receive low-molecular-weight heparin (dalteparin) and half were assigned to receive edoxaban. This treatment continued for up to 12 months. All patients were followed up for 12 months or until study closure (minimum 9 months).
The study was designed to assess two key factors. First, it evaluated whether edoxaban is at least as good as dalteparin with respect to rates of recurrent clots and bleeding, the two main risks associated with treating VTE. Second, it was the first study to measure the benefits of continuing treatment with either drug for more than six months after the initial VTE.
The results confirm that edoxaban is not inferior to dalteparin with respect to composite rates of recurrent clots and bleeding, the trial’s primary endpoint, which occurred in 12.8 percent of those receiving edoxaban and 13.5 percent of those receiving dalteparin. Although edoxaban was associated with a slightly higher rate of major bleeding, this was balanced by a slightly lower rate of recurrent VTE. Analyses of secondary outcomes and subgroups revealed that the two drugs were identical in the rates of the most severe category of major bleeding, and that bleeding was most common in the upper gastrointestinal tract and in patients with gastrointestinal cancers.
“For the vast majority of patients with cancer-associated VTE, treatment with oral edoxaban can replace the injectable dalteparin,” said lead study author Gary E. Raskob, PhD, dean and regents professor of the University of Oklahoma College of Public Health. “Preventing VTE recurrence and major bleeding can allow the oncologist to really focus on the patient’s cancer treatment.”
Raskob added that the results do not necessarily apply to all DOACs because some act through different mechanisms or are metabolized differently than edoxaban. Further studies could elucidate which DOACs might work best in the context of different chemotherapy regimens and also illuminate optimal treatment regimens for those with gastrointestinal cancers, he said.
This study was supported by Daiichi Sankyo.
Gary E. Raskob, PhD, of the University of Oklahoma College of Public Health, will present this study during the Late Breaking Abstracts session on Tuesday December 12, at 7:30 a.m. EST in Hall C2 of the Georgia World Congress Center.
Landmark Trial of Caplacizumab Shows Dramatic Improvements for Acquired Thrombotic Thrombocytopenic Purpura
Results of the Randomized, Double-Blind, Placebo-Controlled, Phase 3 Hercules Study of Caplacizumab in Patients with Acquired Thrombotic Thrombocytopenic Purpura [LBA-1]
In a Phase III trial, patients with acquired TTP, a rare blood clotting disorder, who received the investigational drug caplacizumab showed significant improvements in the time it took to normalization of their platelet count compared to those receiving a placebo. These findings confirm the promising results of previous trials of the drug, which was fast-tracked for FDA review earlier this year.
Acquired TTP (aTTP) is caused by antibodies that block the activity of ADAMTS-13, an enzyme that that cleaves von Willebrand Factor (vWF), a key protein involved in blood clotting. The disorder can emerge suddenly, is associated with a high mortality, may last for weeks, and can recur. During an acute aTTP episode, small clots form that deprive tissues of oxygen. This can lead to organ damage and in severe cases to stroke or heart attack.
If aTTP is left untreated, about 90 percent of patients will die within 30 days of the acute presentation, when the platelet count is at its lowest and the condition most active. Standard treatment consists of exchanging the patient’s plasma with donated plasma and immunosuppression therapy to remove the antibody-producing cells. While this regimen is effective in clearing the harmful antibodies and replenishing the missing ADAMTS-13 enzyme, it can take over 10 days for a patient to realize the treatment’s full effect, during which time he or she can die from a stroke or other complications while waiting for the antibodies to clear.
Caplacizumab is designed to prevent further clots forming during an acute aTTP episode. The drug aims to reduce the immediate risks and prevent organ damage while the standard treatments are used to resolve the underlying disease.
The trial enrolled 145 patients suffering acute episodes of aTTP. All patients received standard of care, including plasma exchange and steroids until resolution of the episode, and could have received monoclonal antibody therapy (rituximab) or further immunosuppressive therapy per investigator practice. In addition, half of the patients were randomized to receive caplacizumab, and the other half received placebo. The first administration of caplacizumab was given intravenously, before plasma exchange. Subsequent daily doses were given subcutaneously for the duration of the daily plasma exchange, and 30 days thereafter, and treatment could be extended for up to an additional 4 weeks maximum if the underlying disease was still ongoing. All patients were monitored for safety for at least 28 days after their treatment ended.
Patients randomized to receive caplacizumab were, at any time point during the study, 1.55 times more likely than those in the placebo group to achieve platelet count normalization. Furthermore, those receiving caplacizumab showed a 74 percent lower risk of a composite of TTP-related death, recurrence, or a major thromboembolic event (such as stroke) while undergoing treatment, and a 67 percent lower risk of experiencing an aTTP recurrence during the entire study period. Those receiving caplacizumab also showed greater responsiveness to treatment, faster normalization of organ damage markers compared to the placebo group, and only minor side effects, such as nosebleeds, bleeding of the gums, and bruising.
Patients receiving caplacizumab also saw a significant reduction in the number of days they required plasma exchange (38%), time spent in the intensive care unit (65%), and overall time spent in the hospital (31%). These reductions suggest the drug could have significant financial implications for treatment of aTTP, researchers said.
“This is a real game-changer in the way we treat patients with aTTP,” said lead study author Marie Scully, MD, a consultant at University College London Hospitals NHS Trust who specializes in TTP. “Caplacizumab is a treatment that offers protection during the most acute, risky period of this disease and bridges the time one has to wait for the inhibitory autoantibody levels to be cleared. It is very beneficial for patient outcomes and is an important addition to the therapeutic armamentarium for clinicians and the hospital.”
This study was supported by Ablynx, NV.
Marie Scully, MD, of the University College London Hospitals NHS Trust, will present this study during the Late Breaking Abstracts session on Tuesday December 12, at 7:30 a.m. EST in Hall C2 of the Georgia World Congress Center.
Trial Supports Addition of Monoclonal Antibody Daratumumab to Standard Treatment Regimen for Patients with Multiple Myeloma
Phase 3 Randomized Study of Daratumumab Plus Bortezomib, Melphalan, and Prednisone (D-VMP) Versus Bortezomib, Melphalan, and Prednisone (VMP) in Newly Diagnosed Multiple Myeloma (NDMM) Patients (Pts) Ineligible for Transplant (ALCYONE) [LBA-4]
The first randomized trial to evaluate the use of a monoclonal antibody drug for treating newly diagnosed multiple myeloma shows that adding the drug, daratumumab, to one of the standard treatment regimens reduced the likelihood of disease progression or death by 50 percent. The regimen also induced significantly deeper response and higher rates of negative minimal residual disease (MRD). The Phase III trial, conducted in patients who were not eligible for a stem cell transplant, suggests daratumumab is a beneficial addition to one of the current first-line therapies for these patients.
Multiple myeloma is a cancer that starts in plasma cells, a component of the immune system. Stem cell transplantation is used as intensification therapy in young patients. For people who cannot receive a stem cell transplant, one standard treatment involves two chemotherapy drugs, bortezomib and melphalan, together with the steroid prednisone. Daratumumab is a newer drug designed to directly target tumors while also equipping a patient’s own immune cells to attack the cancer cells. It is approved for patients whose myeloma has relapsed after an initial course of treatment.
“Our results support that daratumumab in combination with bortezomib, melphalan, and prednisone should become a new standard of care in transplant-ineligible multiple myeloma patients,” said senior study author Jesus F. San-Miguel, MD, Medical Director of the Clínica Universidad de Navarra in Pamplona, Spain. “Monoclonal antibodies like daratumumab have already been approved for use in relapsed patients; here, we are showing that the benefits extend to newly diagnosed patients, as well.”
The trial enrolled 706 patients. All received nine 6-week cycles of the standard treatment regimen. Half were randomly assigned to receive daratumumab along with the standard treatment and continued taking daratumumab once a month after the first nine treatment cycles. To date, patients have been tracked for a median of 16 months.
In terms of the study’s primary endpoint, progression-free survival, patients receiving daratumumab showed a significantly (50%) lower rate of disease progression or death compared to those receiving standard treatment alone, a benefit that was consistent across all demographic and biologic subgroups. This improvement appeared to be largely driven by a significantly better responsiveness to therapy, a higher rate of complete remission, and a tripling of the proportion of patients reporting MRD negativity.
Both study groups showed similar rates of adverse events with the exception of upper respiratory tract infections and pneumonia, which occurred somewhat more frequently in those taking daratumumab, but the majority of these resolved.
The trial is the first of several ongoing studies to evaluate daratumumab as a front-line treatment for newly diagnosed multiple myeloma to report results.
This study was supported by Janssen Research & Development, LLC.
Maria-Victoria Mateos, MD, PhD, of the University Hospital of Salamanca–Instituto deInvestigación Biomédica de Salamanca, Salamanca, Spain, will present this study during the Late Breaking Abstracts session on Tuesday December 12, at 7:30 a.m. EST in Hall C2 of the Georgia World Congress Center.
Targeted Leukemia Drug Venetoclax Found Superior to Standard Chemotherapy for Broad Range of Patients When Combined with Rituximab
Venetoclax Plus Rituximab Is Superior to Bendamustine Plus Rituximab in Patients with Relapsed/ Refractory Chronic Lymphocytic Leukemia - Results from Pre-Planned Interim Analysis of the Randomized Phase 3 Murano Study [LBA-2]
In a Phase III trial, treatment with the targeted cancer drug venetoclax in combination with rituximab more than doubled the likelihood that patients with chronic lymphocytic leukemia (CLL) would survive for two years without cancer progression compared to treatment with the standard chemo-immunotherapy drug bendamustine with rituximab The study is the first randomized trial to show venetoclax is superior to a standard chemo-immunotherapy regimen and the first randomized study to evaluate the survival benefit of venetoclax in combination with rituximab, according to researchers.
The trial focused on patients who experienced continuing or recurrent CLL after initial cancer treatment. CLL is one of the main types of leukemia (cancers of the white blood cells) and accounts for about a quarter of new cases of leukemia each year.
Leukemia cells survive an abnormally long time by producing proteins that interfere with the normal process of cell death. Venetoclax is designed to hasten the death of leukemia cells by binding to and blocking the activity of one such protein, known as BCL-2. By contrast, bendamustine works by interfering with cancer cells’ DNA. Rituximab is a monoclonal antibody designed to help the body’s immune system recognize and attack leukemia cells.
Venetoclax is approved for use against CLL in the United States and several other countries, but approvals are limited to small subgroups of patients, such as those with a specific genetic abnormality. The present trial, carried out at 109 sites globally, sought to assess the safety and efficacy of venetoclax in a broad patient population.
The trial enrolled 389 patients whose CLL had persisted or recurred after at least one previous course of treatment including chemotherapy. Half of the patients were randomly assigned to a regimen of six monthly doses of venetoclax plus rituximab and half received six cycles of bendamustine plus rituximab. Patients assigned to the venetoclax arm continued to use venetoclax alone for two years or until leukemia returned. To date, researchers have tracked patients for a median of about two years.
The vast majority (84.9%) of patients receiving venetoclax survived for two years without showing evidence of disease progression, compared to just 36.3 percent of those who received bendamustine. Venetoclax also outperformed bendamustine for the trial’s secondary endpoints, which included overall survival and markers of cancer remission. In particular, those on venetoclax were far more likely to achieve MRD clearance, which was achieved in 83.5 percent of those taking venetoclax and 23.1 percent of those taking bendamustine. These results suggest venetoclax could be discontinued after two years with a low risk of recurrence in those patients with a deep remission, researchers said.
“This is the first randomized trial comparing any of the new agents targeted to treat CLL against a standard chemoimmunotherapy program, and it has proved the superiority of the chemotherapy-free approach,” said lead study author John Seymour, MBBS, PhD, director of the Haematology Department at the Peter MacCallum Cancer Centre and Royal Melbourne Hospital, Melbourne, Australia. “It suggests that venetoclax should replace chemotherapy for relapsed/refractory CLL and is suggestive that the combination with rituximab is the preferred manner to use the drug. There is also evidence of eradication of detectable disease that opens the prospect of time-limited therapy in this setting.” While venetoclax was associated with a greater risk of abnormally low white blood cell counts, there was no increase in severe infections or deaths related to this side effect, said Seymour.
The researchers continue to monitor participants to assess long-term survival and disease progression.
This study was supported by Genentech, a member of the Roche Group, and AbbVie.
John Seymour, MBBS, PhD, of the Peter MacCallum Cancer Centre and Royal Melbourne Hospital, will present this study during the Late Breaking Abstracts session on Tuesday December 12, at 7:30 a.m. EST in Hall C2 of the Georgia World Congress Center.
The study authors and press program moderator will be available for interviews after the press conference or by telephone. Additional press briefings will take place throughout the meeting. For the complete annual meeting program and abstracts, visit http://www.hematology.org/annual-meeting. Follow @ASH_hematology and #ASH17 on Twitter and like ASH on Facebook for the most up-to-date information about the 2017 ASH Annual Meeting.
The American Society of Hematology (www.hematology.org) is the world’s largest professional society of hematologists dedicated to furthering the understanding, diagnosis, treatment, and prevention of disorders affecting the blood. For more than 50 years, the Society has led the development of hematology as a discipline by promoting research, patient care, education, training, and advocacy in hematology. ASH publishes Blood (www.bloodjournal.org), the most cited peer-reviewed publication in the field, which is available weekly in print and online. In 2016, ASH launched Blood Advances (www.bloodadvances.org), an online, peer-reviewed open-access journal.
CONTACTS:
Stephen Fitzmaurice, ASH
561-506-6890; [email protected]
Adam Silverstein, FleishmanHillard
917-697-9313; [email protected]