Blood Clots
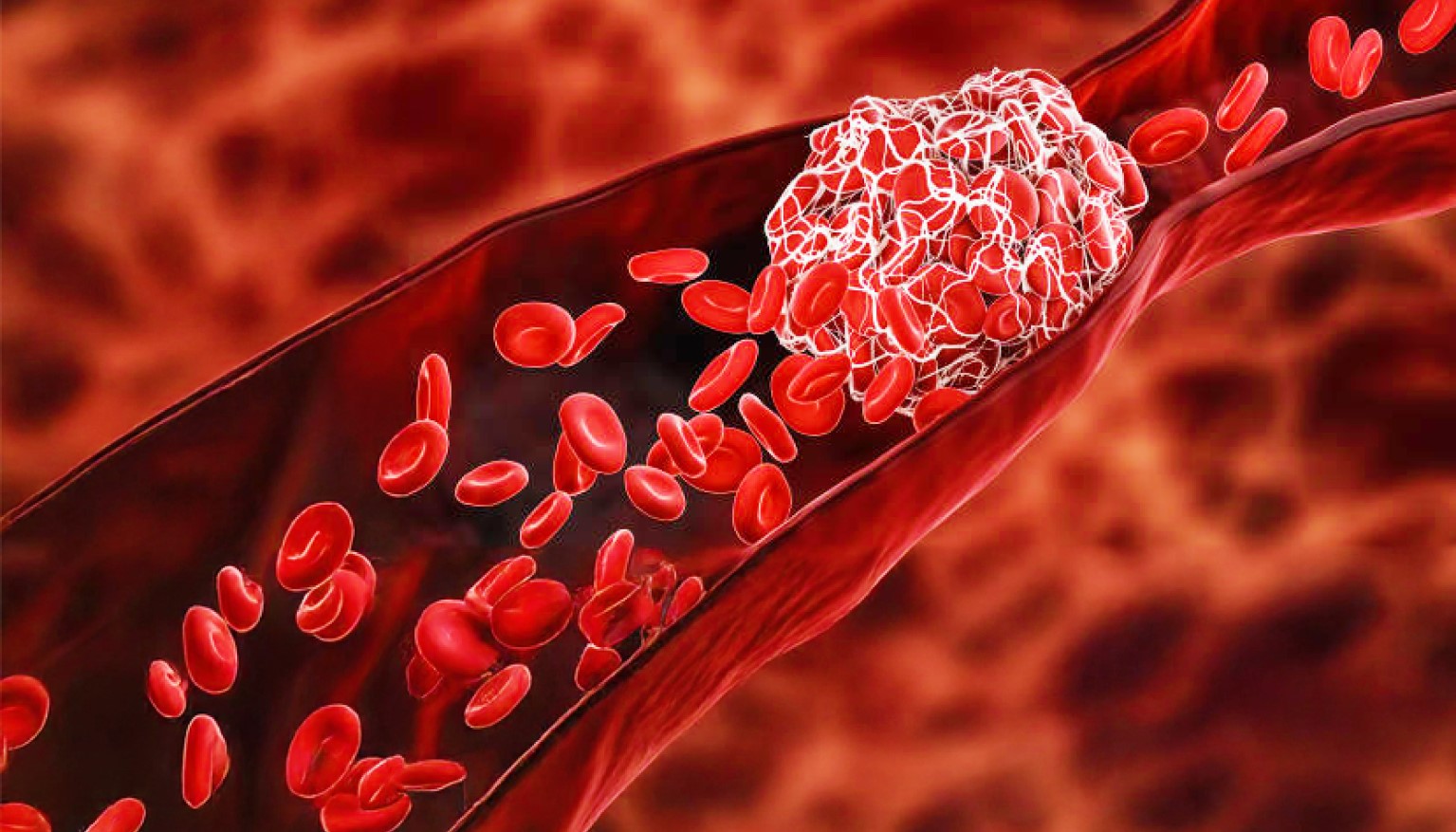
Blood clotting, or coagulation, is an important process that prevents excessive bleeding when a blood vessel is injured. Platelets (a type of blood cell) and proteins in your plasma (the liquid part of blood) work together to stop the bleeding by forming a clot over the injury. Typically, your body will naturally dissolve the blood clot after the injury has healed. Sometimes, however, clots form on the inside of vessels without an obvious injury or do not dissolve naturally. These situations can be dangerous and require accurate diagnosis and appropriate treatment.
Clots can occur in veins or arteries, which are vessels that are part of the body's circulatory system. While both types of vessels help transport blood throughout the body, they each function differently. Veins are low-pressure vessels that carry deoxygenated blood away from the body's organs and back to the heart. An abnormal clot that forms in a vein may restrict the return of blood to the heart and can result in pain and swelling as the blood gathers behind the clot.
Deep Vein Thrombosis
Deep vein thrombosis (DVT) is a type of clot that forms in a major vein of the leg or, less commonly, in the arms, pelvis, or other large veins in the body. In some cases, a clot in a vein may detach from its point of origin and travel through the heart to the lungs where it becomes wedged, preventing adequate blood flow. This is called a pulmonary (lung) embolism (PE) and can be extremely dangerous.
It is estimated that each year DVT affects as many as 900,000 people in the United States and kills up to 100,000. Despite the prevalence of this condition, the public is largely unaware of the risk factors and symptoms of DVT/PE. Do you understand your risk?
Blood Clots in the Arteries
Arteries, on the other hand, are muscular, high-pressure vessels that carry oxygen- and nutrient-rich blood from the heart to other parts of the body. When your doctor measures your blood pressure, the test results are an indicator of the pressure in your arteries. Clotting that occurs in arteries is usually associated with atherosclerosis (hardening of the arteries), a deposit of plaque that narrows the inside of the vessel. As the arterial passage narrows, the strong arterial muscles continue to force blood through the opening, and the high pressure can cause the plaque to rupture. Molecules released in the rupture cause the body to overreact and form an unnecessary clot in the artery, potentially leading to a heart attack or stroke. When the blood supply to the heart or brain is completely blocked by the clot, a part of these organs can be damaged as a result of being deprived of blood and its nutrients.
Am I at Risk?
The risk factors for developing a venous clot are different from those for an arterial clot, and people at risk for getting one are not necessarily at risk for getting the other. Different risk factors or events can cause unnatural clotting; however, each factor may initiate clotting in a different way. There are molecules in your system that signal your body to let it know when, where, and how quickly to form a clot, and genetics plays a role in how quickly your body reacts to these signals. Certain risk factors, such as obesity, slow the flow of blood in the veins, while others, such as age, can increase the body's natural ability to clot. Even certain medications can affect how quickly your blood clots.
The following factors increase your risk of developing a blood clot:
- Obesity
- Pregnancy
- Immobility (including prolonged inactivity, long trips by plane or car)
- Smoking
- Oral contraceptives
- Certain cancers
- Trauma
- Certain surgeries
- Age (increased risk for people over age 60)
- A family history of blood clots
- Chronic inflammatory diseases
- Diabetes
- High blood pressure
- High cholesterol
- Prior central line placement
Blood Clotting and Pregnancy
Blood Clots and Travel
Can Taking Hormonal Birth Control Cause Blood Clots?
Hormonal birth control containing estrogen carries a very low risk of blood clots for most people. While true that hormonal birth control containing estrogen can increase the risk of blood clots, this increased risk remains low – on average, only three to nine out of every 10,000 women taking hormonal birth control pills will develop a blood clot. In fact, the risk of developing a blood clot while on hormonal birth control is significantly lower than the risk while pregnant or after giving birth. For those who stop taking hormonal birth control, research suggests that the increased risk of blood clots largely returns to normal within two to four weeks. Progestin-only methods like hormonal IUDs and mini-pills do not carry an increased blood clot risk because they contain no estrogen.
Individuals with a personal or family history of blood clots, high blood pressure, smoking, or heart problems may not be a good fit for hormonal birth control containing estrogen. Most people don’t have any medical reason to avoid hormonal birth control, but you should always discuss personal and family health conditions with your doctor to reduce your risk.
Find additional trustworthy information on blood disorders in the full Blood Health Information Hub library. Have you seen any misinformation on blood disorders you want ASH to address? Contact [email protected].
What are the Symptoms of a Blood Clot?
In addition to knowing your risk factors, it is also important to be aware of the symptoms of blood clots, which vary depending upon where the clot is located:
- Heart: Chest heaviness or pain, discomfort in other areas of the upper body, shortness of breath, sweating, nausea, light-headedness
- Brain: Weakness of the face, arms or legs, difficulty speaking, vision problems, sudden and severe headache, dizziness
- Arm or Leg: Sudden or gradual pain, swelling, tenderness and warmth
- Lung: Sharp chest pain, racing heart, shortness of breath, sweating, fever, coughing up blood
- Abdomen: Severe abdominal pain, vomiting, diarrhea
How Are Blood Clots Treated?
Blood clots are treated with a plan that takes into account the type of clot, how it happened (risk factors) and a patient’s other specific health situation. If you are experiencing symptoms and suspect you may have a blood clot, see a doctor immediately.
There have been many research advances that have improved the prevention and treatment of blood clots. Almost every patient diagnosed with a blood clot is treated with anticoagulants (blood thinners) to prevent the clot from growing and spreading and to prevent additional new clots from forming. In very specific situations, other treatments can be used such as:
- Anticoagulants: Medicine that prevents clots from forming
- Thrombolytics: Medicine that dissolves blood clots
- Catheter-directed thrombolysis: A procedure in which a long tube, called a catheter, is surgically inserted and directed toward the blood clot where it delivers clot-dissolving medication
- Thrombectomy: Surgical removal of a clot
If you are diagnosed with a venous clot, your doctor may refer you to a hematologist, a doctor who specializes in treating blood diseases. People diagnosed with arterial disease who are at risk for developing a clot in their arteries may have several doctors involved in their care, including a cardiologist (a doctor who specializes in conditions of the heart), a neurologist, and possibly a hematologist.
For some patients, participating in a clinical trial provides access to novel therapies. If diagnosed, you can talk with your doctor about whether joining a clinical trial is right for you.
Are Blood Clots Preventable?
Blood clots are among the most preventable types of blood conditions. There are several ways to decrease your chances of developing a blood clot, such as controlling your risk factors when possible. If you think you may be at risk because of genetic or behavioral factors, talk with your doctor. Also, make sure your doctor is aware of all the medications you are taking and any family history of blood clotting disorders.
Where Can I Find More Information?
If you are interested in learning more about blood diseases and disorders, here are a few resources that may be helpful.